Achromatopsia
By Lori Passarelli ABO-AC FNAO
Release Date: February 1, 2022
Expiration Date: November 1, 2024
Learning Objectives
Upon completion of this course you should understand:
- Identify some of the symptoms of achromatopsia and how the eye processes and perceives color.
- Gain a greater understanding of the properties of light and color.
- Skillfully design a pair of glasses for people with achromatopsia and understand how tinted lenses alleviate its symptoms.s
Course Description
In this course you will learn about achromatopsia a genetic conditions characterized by color blindness, low vision, extreme light sensitivity (day blindness) and nystagmus. We will review the symptoms and and treatments in particular lens options that the ECP can offer the achromat to ameliorate some symptoms and improve visual acuity.
Faculty/Editorial Board
 Lori Passarelli ABO-AC FNAO
Lori Passarelli ABO-AC FNAO
Lori's father, an ophthalmologist, taught her to use the lensometer when she was 14, spawning a lifetime interest in optics and eye anatomy. Since 1998 Lori has managed the optical department at Orange Coast Eye Center, an ophthalmology practice in Fountain Valley, California. Lori is a lifelong learner with an affinity for physics and optics. She is passionate about helping patients select fabulous frames that make them feel good.
TO EARN CONTINUING EDUCATION CREDIT
This course has been approved for one (1) hour of Technical Level III continuing education credit by the ABO. To earn ABO credit, please review the questions and take the test at 2020mag.com/ce. Note: As of January 2020, no tests will be graded manually. Please call (800) 825-4696 for more information.
WHAT IS ACHROMATOPSIA?
Imagine a world devoid of color where everything is black and white or shades of gray. A colorless world might seem incredulous to those with normal color vision, but a colorless world is a reality for those with achromatopsia.
What is achromatopsia? First, let us break down the word to the root definition: The prefix “a” denotes absence, chroma means color, and “autopsia” means blindness. Put them together, and achromatopsia translates to colorblindness. An estimated one in 30,000 people are born with achromatopsia (also called rod monochromatism), an autosomal recessive genetic disorder. The parents of a person with an autosomal recessive disease carry one copy of the mutated genes and are asymptomatic to the condition. A child inheriting a mutated gene from each parent is born with the disorder. (aapos.org/glossary/achromatopsia)
 A person with achromatopsia cannot see color because their cone photoreceptor cells are dysfunctional. Human vision is primarily the result of images formed by the foveal cone photoreceptor cells, but achromats lack functional cones including foveal cones needed for sharp central vision and photopic (daylight) vision. Instead, they rely solely on rod photoreceptors to see. However, rods do not differentiate wavelengths; therefore, they cannot produce a color signal, only shades of gray, black and white. Achromatopsia has two types: complete with no functional cone cells and incomplete achromatopsia that have functional rod cells, and one type of functional blue cone cell to varying degrees. However, it is complete achromatopsia that is the most severe with more adverse visual symptoms. There is no cure for achromatopsia, but some clinical studies show promising results with gene replacement therapy, specifically for CNGA3 and CNGB3-related achromatopsia, in restoring cone function in dogs and mice.
A person with achromatopsia cannot see color because their cone photoreceptor cells are dysfunctional. Human vision is primarily the result of images formed by the foveal cone photoreceptor cells, but achromats lack functional cones including foveal cones needed for sharp central vision and photopic (daylight) vision. Instead, they rely solely on rod photoreceptors to see. However, rods do not differentiate wavelengths; therefore, they cannot produce a color signal, only shades of gray, black and white. Achromatopsia has two types: complete with no functional cone cells and incomplete achromatopsia that have functional rod cells, and one type of functional blue cone cell to varying degrees. However, it is complete achromatopsia that is the most severe with more adverse visual symptoms. There is no cure for achromatopsia, but some clinical studies show promising results with gene replacement therapy, specifically for CNGA3 and CNGB3-related achromatopsia, in restoring cone function in dogs and mice.
Without a cure, reducing or alleviating symptoms of the disease to help a person function in daily life more comfortably is imperative. As opticians, we play a role in the treatment plan by ordering glasses or contact lenses suitable to this end.
THE VISUAL SYSTEM
Given that achromats only have rod vision, let’s review the normal visual system versus rod only mediated vision. Our eyes are remarkable self-contained organs capable of producing images and color signals that the brain interprets as visual perception. Lining the back
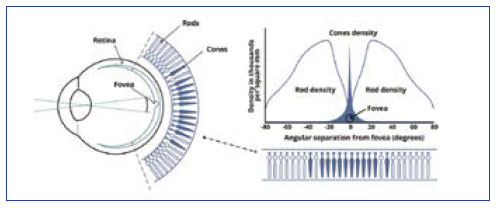
of the eye’s globe is the retina, with two types of photoreceptor cells: rods and cones. We have an estimated 6 million cones concentrated mostly in the central retina and 100 million rods concentrated more in the peripheral retina. These photoreceptive cells convert incident light energy to signals that enter the optic disc, a blind spot made of nerve cells, before traveling the visual pathway, crossing at the optic chiasm and ultimately arriving at the visual cortex of the brain where the perception of sight occurs.

Rod photoreceptor cells are 500 to 1,000 times more sensitive to light than cones, but they are only active in low light conditions and do not produce color signals or high-resolution images. Rod cells allow us to see in scotopic conditions and provide dark-adapted vision. For example, if we are in a dark room, our rods are able to detect minuscule amounts of light to help us see in see in the dark, but the cones are inactive in the dark, so we do not see color. Rod cells do not contribute to high-resolution vision as their numbers are low in the macula, and the central fovea contains none. However, rods are present at a higher ratio than cone cells in the peripheral retina, and therefore aid in peripheral vision. Rod cells contain a photosensitive pigment called rhodopsin. Activation of a single unit of rhodopsin amplifies rod stimulation, causing a significant reaction; in other words, rods have a large response to a small amount of light. A single photon of light can activate a rod cell, while it takes tens to hundreds of photons to activate cone cells. The supersensitivity of rod cells to light comes at a cost as multiple rod cells pool together to converge on a single interneuron, resulting in a low-resolution image. The response rate to light is also slower in rods, making quick visual adjustments less accurate than cone-activated sight.
Conversely, our three types of cones fire under photopic (daylight) conditions and contain pigments enabling us to see color. Cone cells mostly congregate in the macula, and most specifically, the fovea centralis, a 0.3 mm diameter area in the macula’s center. The fovea produces the sharpest vision and color vision because of the high concentration of cones and lower convergence rate. An average of six cone cells converge on a single ganglion cell, while a single foveal cone cell converges on a single ganglion cell (1 to 1). Hence, the highest resolution and color perception occurs from foveal cone signals. Rods produce low-resolution signals because an average of 120rod cells converge on a single ganglion cell, and rod cells are absent from the central fovea. (courses.washington.edu/psy333/lecture_pdfs/ Week2_Day3.pdf)
Ganglion cells are neurons that process and carry information from retinal photoreceptor cells to the brain via the optic nerve; in fact, the optic nerve is made up of the long axons of the retinal ganglion cells. Three cone types are activated by long, medium or short wavelengths: red, green or blue light. Spectral sensitivity within the three types of cones varies. Each type of cone cell contains conopsin, a pigment that activates when light is absorbed. The sensitivity of normal color vision depends on the overlap between the absorption ranges of the three cone types: In other words, we see different colors as different cones stimulate to varying degrees. Any number and combination of cone types can fire in unison, and it is in this, the human eye can perceive an estimated 10 million colors.
Understanding how rod and cone cells respond differently to light helps us imagine how people with achromatopsia see without functional cones needed for color vision. Achromats suffer from more than color blindness. They also experience painful light sensitivity and an aversion to light and glare in bright light conditions that overwhelm the light sensitive rod cells. Achromats suffer from partial or complete lack of central vision and a delayed response to image change. The achromat’s vision is limited or absent in bright light. Singer/songwriter Caitlin Smith describes her visual experience: “My vision is like an out of focus, over-exposed black and white film. And if it’s a sunny day out there, it will be completely over-exposed; I’ll only see white.”
Molecules that make up the objects in our environment either absorb or reflect wavelengths of light, dictating which colors we perceive. The colors we see are a response to the reflected wavelengths from 400 to 700 nm defined as visible light spectrum. In other words, when looking at a ripened lemon in the daytime, the blue and violet waves are absorbed, and the red and green waves are reflected. Reflected light waves excite their corresponding cone photoreceptor cells, and electrochemical signals are generated that ultimately travel through the optic nerve to the visual cortex of the brain, where they are processed.
Thus, we perceive the lemon as yellow. Conversely, in a dark environment, only rods would activate, and the lemon would appear a shade of white or gray. Technically light is not colored. Light is an electromagnetic wave with a specific wavelength or combination of wavelengths; it has no color but the wavelengths incident on the retinal cones produce signals that our brain interprets as color. An object emitting or reflecting light to our eye appears to have a specific color due to the eye-brain response to the wavelength. So technically, there is no such thing as yellow light. Instead, there is light with a wavelength of about 590 nm that appears yellow. Moreover, light with a mixture of wavelengths of about 700 nm and 530 nm appears yellow. The yellow appearance of these two different light sources can be traced to the physiological and psychological response of the eye-brain system and not to the light itself. A person with achromatopsia has no functioning cones for color vision and would see the lemon as a shade of gray or white in both light and dark conditions.
Regarding rods and cones, the different photo pigments (opsins) in our photoreceptor cells each exhibit peak spectral sensitivity to different wavelengths in the visible spectrum. The human eye is most sensitive to a wavelength near 555 nm in daylight (photopic) conditions but shifts to a maximum spectral sensitivity of 507 nm in dark (scotopic) conditions. Depending on luminance levels, our spectral sensitivity shifts from photopic, mesopic and scotopic. Photopic vision prevails in daylight or bright light environments elicited by the excitatory response of all three cone opsins. Scotopic vision is rod-generated vision provoked by dim to low light. Mesopic vision is the state between the two when both rods and cones respond to waning light levels. This shift from photopic to mesopic vision occurs when the peak luminance sensitivity of the eye shifts toward the blue end of the color spectrum as illumination levels decrease. Photoreceptor cells respond to different wavelengths; rods have a peak spectral sensitivity to shorter wavelengths in low illumination while the peak spectral sensitivity of cones are to the longer wavelengths under high luminance levels. The peak sensitivity of rod photo pigments is around 500 nm, and cones show peak sensitivity near 530 nm for green and 560 nm for red. As light levels shift from dark to light or vice versa, our eyes enter into mesopic vision; this in-between state is called the Purkinje effect. The Purkinje effect happens during the transition between cone-based photopic use and the rod-based scotopic system. As light level decreases, the rods take over, and before color disappears, a shift toward the maximum sensitivity to rods occurs. During this shift, cones pool with the more light sensitive rods, sufficient light is present to elicit a response for the red, green and blue cones so both the cones and rods work together in mesopic conditions. It is interesting to note that achromats don’t experience the Purkinje effect since their rod cells mediate the threshold in both photopic and scotopic light environments.
In the 1950s, George Wald, a biochemist, established that the absorbance of light by retinal pigments corresponded to the different wavelengths that activated photoreceptor cells. By using a spectrophotometer, Wald demonstrated that rods are most sensitive to wavelengths near 498 nm (green-blue) and least sensitive to longer wavelengths around the 640 nm (red) range. His research also showed that vitamin A played a vital role in proper retinal function. Wald won the noble prize in Medicine or Physiology in 1967 for his research into the chemistry of vision.
SYMPTOMS AND TREATMENT OF ACHROMATOPSIA
 Parents arrive at the ophthalmologist’s office with their infant, concerned and confused by their child’s “shaking” or “quivering” eyes. Nystagmus is usually the first outward symptom parents notice. Parents may also report their child’s intolerance to daylight. Achromats have Hemeralopia or day blindness. They experience debilitating glare and report extreme pain when exposed to daylight. Pupil constriction in the dark is another sign of achromatopsia. Considering rod photoreceptor cells’ high sensitivity to light and the high level of convergence on ganglion cells, and that the patient with achromatopsia relies solely on rods for vision, it is easier to imagine the blinding effects of hemeralopia. Achromatopsia is usually evident by about six months of age due to the symptoms hence described. The ophthalmologist will take a family history during the examination and perform nystagmus and visual acuity test during the medical visit. In older children, color plate tests may include the Ishihara pseudoisochromatic tests, the City University tests and the Farnsworth panel D15 color test. If achromatopsia is suspected, the doctor may order optical coherence tomography, fundus autofluorescence, visual fields and electroretinogram. The doctor may also recommend genetic testing to confirm the diagnosis.
Parents arrive at the ophthalmologist’s office with their infant, concerned and confused by their child’s “shaking” or “quivering” eyes. Nystagmus is usually the first outward symptom parents notice. Parents may also report their child’s intolerance to daylight. Achromats have Hemeralopia or day blindness. They experience debilitating glare and report extreme pain when exposed to daylight. Pupil constriction in the dark is another sign of achromatopsia. Considering rod photoreceptor cells’ high sensitivity to light and the high level of convergence on ganglion cells, and that the patient with achromatopsia relies solely on rods for vision, it is easier to imagine the blinding effects of hemeralopia. Achromatopsia is usually evident by about six months of age due to the symptoms hence described. The ophthalmologist will take a family history during the examination and perform nystagmus and visual acuity test during the medical visit. In older children, color plate tests may include the Ishihara pseudoisochromatic tests, the City University tests and the Farnsworth panel D15 color test. If achromatopsia is suspected, the doctor may order optical coherence tomography, fundus autofluorescence, visual fields and electroretinogram. The doctor may also recommend genetic testing to confirm the diagnosis.
Visual acuity in achromatic children is poor and generally measurable at 20/200 or less. Corrective lenses help but will not restore normal vision. Children with incomplete achromatopsia may have better vision (20/120 to 20/80) and fewer visual symptoms. Most refractive errors show the need for high plus powered lenses to correct hyperopia. Achromatopsia is a non-progressive disorder, which means the vision is usually stable over time.
Maximizing visual acuity and comfort for patients with achromatopsia is imperative, and opticians play a role in this objective by designing appropriate lenses. Controlling the amount of light entering the eye is crucial in helping achromats manage their extreme light sensitivity. Achromats rely solely on rod vision, and as we’ve learned, rods only function in low-light conditions. In bright light, rod photoreceptor cells bleach out or saturate, causing hemeralopia (white-out). The brighter the light, the faster rods bleach out, causing the white-out effect. Red-colored lenses reduce light sensitivity by blocking the green and blue medium and short-wavelengths while allowing the longer low-energy wavelengths to transmit, reducing rod saturation. Rod cells have low sensitivity to long wavelengths, and it is for this reason that red filtered lenses help prevent retinal bleaching and allow rhodopsin photopigment to recharge to its active conformation. A noticeable self-adapting solution to the discomfort is for the patient to squint or close their eyes to block light. Without lens filters, images appear washed out with little detail or contrast, much like the white-out effect of a blizzard. Red filtered lenses help ameliorate this effect by intensifying the various tones and shades of gray, improving contrast.
Personalized freeform lens designs optimize lens performance to minimize aberrations for improved peripheral vision. For this reason, utilizing a quality freeform lens design for the achromats is the best choice. Providing position of wear measurements to the lab for compensation calculations is essential. Digital freeform lens design optimizes the lens’ visual performance for the individual based on their prescription, material index, base curve and fit parameters. Include the following measurements to achieve this goal: vertex distance, pantoscopic tilt, frame wrap angle, monocular PDs, and OC height. Before taking measurements, adjust the frame and ask the patient to assume their natural posture. Monocular pupillary distance and OC height should be exact and double-checked when working with very young children, as it may be challenging to get the child to sit still long enough to get an accurate measurement.
Two pairs of eyewear are recommended for an achromat; one for outdoors and one for indoors. The outdoor lenses must dramatically reduce visible light transmission since intense light is blinding. The goal is to mimic low light conditions and to use a red filter so that the rod cells the achromat uses even in daylight conditions don’t bleach out from too much light, and a red lens improves contrast sensitivity for the achromat.
While polycarbonate or Trivex is standard for all children, patients old enough to verbalize discomfort may report that lenses made from these materials are not dark enough to control hemeralopia. While the newer polycarbonate lenses absorb dyes better than older versions, CR-39 is known to darken to acceptable levels. CR-39 quickly absorbs tints and has excellent optical performance, with an Abbe value of 59. The material reflects 7.7 percent of visible light from the surface and transmits 10 percent UVA, requiring a UV coating. Trivex lenses afford exceptional optics with an Abbe value of 44, and its specific gravity of 1.11 makes it the lightest of all lens materials, but Trivex does not absorb tint as readily as CR-39.
The decision to use CR-39 lenses is best made after educating the parent, discussing it with the prescribing doctor and ultimately having the guardian sign a consent form detailing the risks of shatter in the event of impact if CR-39 lenses are chosen. Also, inform the patient that CR-39 lenses are not to be used for sports or any situation where there’s a potential for impact injury.
While the indoor glasses may not require a solid number four tint like the outdoor pair, a red number three is still needed. Tint color visible light transmission levels should always depend on patient comfort and feedback. Once establishing the amount of darkness the individual patient prefers, the patient’s glasses can be ordered with visible light transmission levels best suited to the patient’s needs.
Frame selection also plays a role in alleviating the symptoms of glare. Frames with shields on the top and sides or face-forming wraparound frames with wide temples provide the most protection from incoming direct light as well as light entering from the sides and top of the frame. Ideally, choose a frame with a top shield to help block light from entering from above. Frames with a top shield are ideal as they will help block overhead light from entering. Specify on the order form BPI 550 red or BPI Deep Red Monochrome 600. This red-orange to red tint helps alleviate the debilitating glare experienced by achromats.
A quick call to the lab manager to reiterate the need for solid Red #4 dye may reduce the need for a redo. Keep in mind that most lab technicians are not privy to the needs of achromats and their requirement for very dark red lenses, and it is not uncommon for the original order to come back with too-light lenses. For those with complete achromatopsia, red-tinted lenses work best, but for patients with incomplete achromatopsia, a magenta filter allows some blue color to enter the lens, which proves beneficial. People with incomplete achromatopsia or blue cone monochromatic have functioning rods and blue cones but lack the red and green cone function. Using a solid red filter on these patients may block some blue light from reaching the retina, and the patient will lose their residual blue color vision.
The color magenta is composed of both red and blue dyes. Magenta allows red and blue light to pass through to the retina, thereby reducing glare and the bleaching of rod receptor cells; this allows the blue channel to respond, affording the patient to see some semblance of the blue hues better than they would without the magenta filter.
Some children and adolescents may prefer colored contact lenses over glasses due to peer acceptance and social interaction. Both rigid and soft contact lenses are available with a custom red tint or magenta-colored option as required for the individual patient. Red-tinted contacts also aid in reducing high-energy blue light from entering the eye. Wearing wraparound sunglasses over red-tinted contact lenses further reduces light transmission and glare, and is recommended for outdoor use.
Although opticians do not diagnose nor treat medical eye conditions, understanding how the eye functions, the visual system and how we see color helps us comprehend and imagine people’s visual experience with achromatopsia. With this heightened awareness, we can better help people with achromatopsia achieve maximum visual acuity while making the world a more comfortable place to live for those who suffer from the disease. Moreover, we design lenses confidently while showcasing our expertise as competent and knowledgeable professionals.



