Sponsored by Neurolens
Read Neurolens: Relief is in Sight Part 1
By Lori Passarelli, ABO-AC
Google “digital eye strain,” and a whopping 107,000,000 results populate. Type in “computer vision syndrome,” and another 68,400,000 results bombard your screen. Topping the list is a link to The American Optometric Association’s website, where you will discover that the average American worker spends seven hours a day on the computer. But even this figure may be understated.
In a 2021 Ipsos poll conducted on behalf of the New Global Myopia Awareness Coalition (GMAC), children and their parents spend double the time they did pre-Covid staring at digital screens. The poll, conducted to measure the growth rate of myopia in children due to near-focus trends, high- lights the incredible effect that the rapid acceleration of digital device usage is having on our vision.
In Neurolens Relief Is in Sight Part 1, which was featured in the April issue of 20/20’s Pro to Pro series, we discussed trigeminal dysphoria, a syndrome caused by the overstimulation of the fifth cranial nerve during prolonged computer screen use as the eyes attempt to reconcile peripheral and central vision during convergence. This overstimulation causes symptoms associated with Digital Vision Syndrome (DVS), including asthenopia or eye strain, dry or watery eyes, neck and shoulder pain, and headaches.
A Neurolens study of over 160,000 people showed that 2 out of 3 people experience symptoms from eye misalignment. Yet only 1 in 10 people report these symptoms to their eye doctor. The reason is simple: Most people don’t know that their eye doctors might have solutions available. In many ways, doctors are detectives; they must listen intently to the patient, analyze symptoms and ascertain their root causes. Asking the right questions is imperative in identifying trigeminal dysphoria. Often, patients come to the office stating vague complaints such as “my eyes water” or “the computer is blurry.” In particular, patients may not correlate symptoms like dry or watery eyes—or even the sensations of dizzinessor motion sickness—to prolonged computer use. Typically, patients don’t connect symptoms to the cause; they just want their eyes to work and see correctly without discomfort or effort. (FIG. 1)
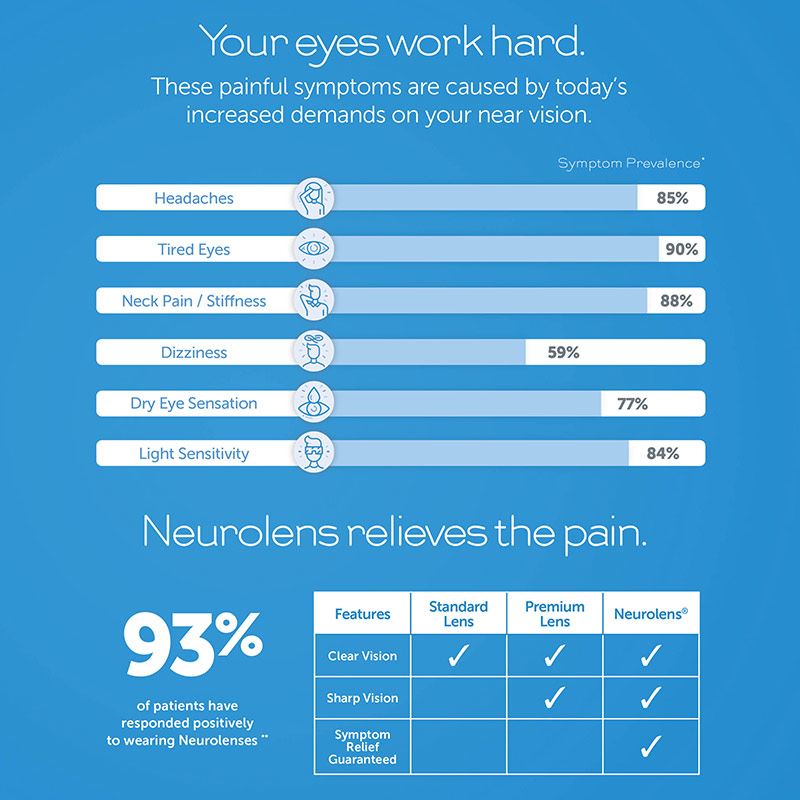
FIG. 1
What a patient doesn’t say is as important as what they do say. For instance, the patient may take their neck complaint (an increasingly common symptom of eye misalignment) to their PCP but not their optometrist. To this end, a questionnaire designed to tease out symptoms of eye misalignment is the easiest way for the patient to denote signs they may otherwise fail to mention to the doctor, thereby aiding in the diagnosis of trigeminal dysphoria. Neurolens has an easy-to-use questionnaire called Lifestyle Index, which is available as both a printed form and an easy-to-complete online screener.
Once the patient symptomology has been ascertained, the Neurolens Measurement Device, Gen 2—or NMD2—tests for these subtle eye misalignments or phorias with an accuracy and consistency unattainable by standard cover tests, which are often subjective and have a higher error rate. The NMD2 starts by measuring pupillary distance (PD) while the patient looks at moving graphics. After determining the PD, a base alignment is performed wherein the system looks for eye turn in the eye that is not presented a target on which to fixate, detecting any dissociated phorias. Then it moves to an associated test or a fine alignment measurement. During this part of the test, the patient sees moving peripheral images as the target alternates centrally between the left and right eye. Eventually, the target adjusts to neutralize any eye movement or fixation disparity. The NMD2 then adjusts its optics to simulate a closer accommodation distance (50 cm) and establishes near pupillary distance during convergence. The device then measures both base and fine alignment at this near distance. The final results confirm monocular pupillary distance and alignment at both near and distance, along with the AC/A ratio. It also detects horizontal and vertical misalignment at both near and distance, which in most cases are different, warranting a contoured prism to correct each one appropriately. The device also provides a recommendation of the prism value that the patient might need to relieve their symptomology known as the Neurolens value. This can be readily used by the doctors as a prescriptive guideline. According to their website, the NMD2 collects thousands of data points per patient and can identify eye misalignment as small as 0.01 Prism Diopters, a level of specificity unmatched by cover tests or other common methods.
The measurements gained by the NMD2 help the doctor accurately diagnose trigeminal dysphoria and prescribe Neurolenses. Available in Single Vision, Office and Progressive designs, Neurolenses employ a customized contoured prism in order to intelligently place the prism power where it’s needed most, effectively addressing the eye misalignment and its corresponding symptoms.
For many practitioners, prescribing prism elicits anxiety; but it shouldn’t. Diagnosing DVS-related trigeminal dysphoria should be standard practice for all patients and incorporated into their annual eye exam. Good vision is not just about clarity; it’s about fusion, binocularity and comfort.













