We see a lot of eye issues every day in this field. Patients with blurry vision who need something as simple as glasses, some who have eye diseases and need a daily regimen of eye drops or ointment for treatment, others who may be referred to a specialist for more extreme treatments. It becomes just another day’s work until it hits close to home. That’s exactly what happened to me.
It begins with a 73-year-old Caucasian female (also known as my mother) with complaints of blurry vision in the right eye for the past month. Over a year ago, she had been diagnosed with 1+ nuclear sclerotic cataracts with very little visual disturbance and mild dry macular degeneration. She was still correctable to 20/20 in both eyes. On this day, her left eye was only correctable to 20/25. No change in the cataract. With retinal photography, we saw a few small flame hemorrhages.
Of course, I tattled on my mom. She had been diagnosed with high blood pressure years ago. A diuretic was prescribed, but due to her job, she was unable to take it. Diuretics are well known to make the takers urinate frequently throughout the day. For a bus driver, that was not an option. Instead of getting anything different prescribed, she just stopped taking it.
Having found the hemorrhages, our next appointment was with a general practitioner to get her blood pressure in check. Unfortunately, this can be a process. My mother had to first find a general doctor. Once I did a ton of research on local doctors, she finally agreed to see one. At the first appointment her blood pressure was 186/98. She blamed it on “white coat syndrome.” I sat in the corner and just waited to see what the doctor’s first step would be. The first medication was prescribed, and a one month recheck scheduled. We returned for the recheck and the blood pressure was still too high, 168/90. Then the second blood pressure medication was prescribed. Finally, after three visits and two blood pressure medications, we have a stable blood pressure, 130/80. That was great news.
 |
Within two weeks I got the phone call from mom that something was wrong. The vision in the left eye was worse. She had gone to take her DOT driving exam but couldn’t pass the vision check. Don’t get me wrong, she has been retired for years and does not need a DOT license, however, I am so glad she went to get it. Upon examination, her left eye’s visual acuity had worsened to 20/50. With retinal photography we found that the flame hemorrhages were gone, but now she had a macular hemorrhage.
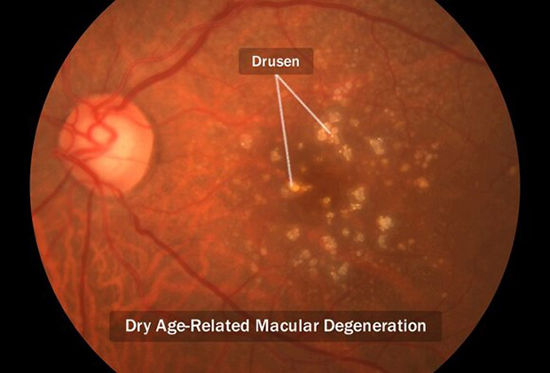
Off to the next referral, a retinal specialist. We happen to have some of the best retinal doctors in the Southeast right across the street from my office. We got in within a few days. Before this appointment I wanted to prepare my mother for what she should expect during her appointment. I skipped a few things, just so she didn’t chicken out. The retinal group and all the employees were amazing. This made my mother a lot calmer, and I will have to say that it helped calm my nerves too. We went in, had an OCT and photos. Once it was pulled up on the screen you could see three elevated areas of swelling and bleeding. The retinal specialist explained that in only a small percentage of patients diagnosed with dry macular degeneration, it turns into the wet form. This is when I found out that my uncle had been diagnosed with it a few years ago. That was one strike against her (family history), her skin color was the second (Caucasians are much more likely to be diagnosed with macular degeneration than any other race), and her issues with elevated blood pressure was the third. Of course, an injection of medication into the eye to reduce the swelling would be the best treatment. Panic engulfed my mother. I played it off like it was nothing. The technicians got her numb. Next thing you know the doctor told her to look over at the wall and within seconds it was over. She was relieved, and so was I.
Three days later my mother was in the area near my office and I had her stop in for a quick visual acuity check - 20/20 already. Simply amazing! But to keep this clarity is an ongoing task. Every 4-6 weeks we will be visiting our wonderful retinal specialist for rechecks and more injections. This is a forever treatment, not just six months or a year. This is for the rest of her life.
Now that numb feeling I used to have for patients has turned into understanding the fear and worry not only for the patient but for the family. I feel like I do a better job now with giving explanations and preparing others for what may be in store. It is a realization, but in a great way. I know what it’s like to be that person sitting in the corner chair anxiously waiting to get results for a loved one and knowing what the stakes are. It brings a different outlook on my job and all the jobs of healthcare providers. We do get overworked, in many cases underpaid, and every day underappreciated, but keep pushing to do your best and always try to see problems from the patient’s and family’s perspective. You can make a difference and not even realize it.
Learn about age-related eye diseases and how nutrients can aid in postponing and minimizing their effects with our CE, Nutrition and Vision, at 2020mag.com.












