US Pharm.
2006;31(9):20-34.
Urinary
incontinence (UI) can have a negative impact on an individual's quality
of life by lowering self-esteem and affecting psychological and physical
well-being. According to a study supported in part by the Agency for
Healthcare Research and Quality, elderly Americans who are incontinent often
experience shame, disgust, embarrassment, and a less active social life, all
of which can lead to depression.1 Furthermore, elderly individuals
with UI are more likely than those without it to have symptoms of depression.
1
According to a recent survey,
called What Older Women Want, women ages 55 to 95 rated UI as number 5
among the top 10 unmet health priorities.2 This finding is
consistent with previous data showing that elderly women express more concerns
about living with disabilities than developing common illnesses.2
Despite these findings, UI is underdiagnosed and often underreported by
patients due to embarrassment or acceptance of the condition as a consequence
of aging, although it is not actually caused by aging.3,4
This article encourages
pharmacists to raise awareness of UI, educate patients about the condition,
and provide appropriate recommendations for treatment. By approaching UI as a
condition with underlying, though sometimes irreversible causes, pharmacists
can help manage patients well enough to improve symptoms and minimize
complications.5
Prevalence
UI affects
approximately 17 million Americans, including more than 50% of seniors in
hospitals or nursing facilities and 8% to 34% of community-dwelling seniors.
6,7 It is especially prevalent in women, with a greater than 45%
occurrence in those ages 50 to 59.8 Overall, data show that 17% to
55% of elderly women versus 11% to 34% of elderly men are affected.9
UI leads to decreased quality of life in up to 44% of affected women.2
Furthermore, the presence of UI is a predictive factor for nursing home
admission.9,10 One study found that the prevalence of depression
was 15.5% in women with UI, compared with only 9.2% in women without UI.11
Management of UI presents a significant financial strain on patients, health
care facilities, and industry and government agencies providing health care
funding, incurring a direct annual cost of $26.5 billion.12
Continence and UI Complications
Normal urination is
a complex process, requiring both a bladder that can store and expel urine and
a urethra that can close and open appropriately. Normal micturition occurs
when bladder contraction is coordinated with urethral sphincter relaxation.
Additional factors necessary for continence are related to a patient's
cognitive function, dexterity, social awareness, motivation, and locomotive
ability. The central nervous system integrates control of the urinary tract.
The inability to control urination in a socially appropriate manner is known
as UI.
Complications associated with
UI include skin rashes, pressure ulcers, and indirectly, falls and fractures.
Use of an indwelling catheter is associated with patient discomfort, use of
drugs for bladder spasms, and an increased risk of life-threatening
infections, bladder stones, and cancer.13 Decreases in sleep,
social interaction, and self-esteem can affect psychological well-being. In
addition, family members and health care facility staff who care for a
functionally dependent patients with UI may experience increased levels of
stress.
Diagnostic Assessment
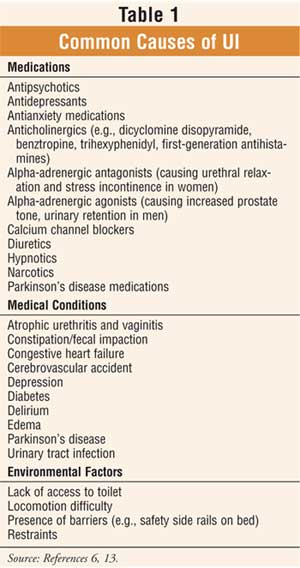
Distinguishing
which type of UI a patient has is critical for prescribing the appropriate
treatment; this begins with determining the cause of UI (TABLE 1). This
process comprises a thorough physical examination as well as an evaluation of
the patient's medical history. This would include an evaluation of the
patient's medication history to rule out reversible medication-related causes
of UI. Pharmacists should have an active role in the assessment process, since
UI due to anticholinergic, narcotic, and beta-adrenergic drugs can be improved
by switching or discontinuing medication or modifying the dosage schedule when
appropriate.3 The pharmacist's expertise can prove to be a valuable
addition to the team approach of increasing quality of life and decreasing
cost of care.14
The physical exam should
assess the patient's medical condition as well as cognition, dexterity, and
mobility. An examination of the abdomen, genitals, pelvis, and rectum should
also be conducted. Edema and neurologic abnormalities may contribute to UI
and, therefore, should be ruled out. Since it may be difficult to correctly
diagnose UI, patients should also be examined for urinary tract infection,
post-void residual volume, and simple cystometry measures of bladder capacity
and stability.3 Detecting potentially reversible causes of UI
should always be a priority. Urodynamic instruments such as a uroflowmeter and
cystometer should not be used as screening tools, because results of these
tests do not differ significantly for continent and incontinent patients;
however, using these tools as confirmatory tests may help to determine a
therapeutic approach.3
Classifications
There are a number
of different types of UI, and more than one type may be present simultaneously
or overlap with one another.
Stress Incontinence
Stress incontinence
is common among senior women, especially in ambulatory clinic settings.
15,16 It is usually associated with weakened supporting tissue, which
results in hypermotility of the urethra and bladder outlet.15
Coughing, sneezing, laughing, exercising, or any other physical activity that
increases intra-abdominal pressure may cause uncontrolled urination.15,17
Symptoms can be infrequent, with small amounts of urine and no need for
specific treatment, to severe and bothersome, necessitating surgical
correction.16 Vaginal childbirth, estrogen de ficiency, obesity,
and/or surgery can contribute to stress incontinence. While stress
incontinence is rare in men, it can occur in such patients after transurethral
surgery and/or radiation therapy for lower urinary tract malignancy (e.g.,
prostate cancer) when the anatomic sphincters are damaged.16
Urge Incontinence
The most common
type of UI among those age 85 or older is urge incontinence, which is caused
by abnormal involuntary detrusor muscle contractions (i.e., detrusor
overactivity).18,19 It is characterized by an abrupt, strong desire
to urinate as well as frequent urination (e.g., more than every two hours) and
nocturia.16 Patients may lose urine on their way to the toilet, and
some may experience a degree of urinary retention. Causes of urge incontinence
include central nervous system disorders (e.g., stroke, dementia,
parkinsonism, spinal cord injury) and lower genitourinary conditions (e.g.,
tumors, stones, diverticula, outflow obstruction).16 It is possible
that symptoms of urge incontinence among the el derly may be misinterpreted
as agitation related to a behavioral disturbance secondary to dementia.
Overflow Incontinence
Overflow incontinence occurs from distention of the bladder as a result of an inability to empty normally. It is the most common form of incontinence among elderly men. Symptoms include frequent urination, urgency, dribbling, urge incontinence, and stress incontinence. Causes of overflow incontinence vary and include uterine prolapse, urethral strictures, prostate enlargement, diabetes, and spinal cord injury.18
Mixed Incontinence
Mixed incontinence
occurs in 50% to 60% of patients with UI and is characterized by symptoms of
both urge incontinence and stress incontinence.20 It is most
commonly seen among older women. Mixed incontinence is also commonly seen as a
combination of urge and functional incontinence among nursing home residents.
15
Functional Incontinence
Functional
incontinence may be caused by cognitive impairment, psychological impairment,
impaired mobility, medications, or dexterity problems that render the patient
unable or unwilling to toilet properly.6,17 For example, delirium
promotes incontinence by increasing disorientation and decreasing patient
awareness of the need to void. Mobility impairment affects the ability to
reach the toilet in time.3 Functional UI may exacerbate other types
of persistent incontinence.15
Complex History of UI
Incontinence
associated with pain, hematuria, recurrent infection, pelvic complications
(e.g., bladder cancer, bladder stones, prostate cancer), herniated disks, and
metastatic tumors is classified as complex history of UI. This type of UI
usually requires a specialized management approach.13,21
Management of UI
Treatment options
for the management of UI include both nonpharmacologic and pharmacologic
therapy.3
Nonpharmacologic
Intervention
Nonpharmacologic
therapy is recommended in conjunction with pharmacotherapy. Nonpharmacologic
interventions that are helpful in the management of UI include--but are not
limited to--behavior modifications such as bladder control training and dietary
modification, prompted voiding, and use of absorbent products and catheters.
Behavior modification, used
alone or in combination with other treatment modalities, is safe, effective,
and the least invasive treatment for UI.17,22,23 Bladder control
training can be useful for managing UI. Kegel exercises, which involve
alternating contraction and relaxation of the pubococcygeus muscle, improve
pelvic floor muscle tone and help the bladder store urine for longer periods
of time. Patients should begin by performing 10 alternating three-second
contractions and relaxations per day and gradually increase to 80 to 150
10-second contractions and relaxations per day.2 In some cases,
biofeedback and electrical stimulation may be recommended in conjunction with
pelvic floor exercises to help control urge and overflow incontinence.24
Another method of bladder control training, known as bladder retraining
, involves gradually increasing the time between voiding by 15-minute
increments each week until voiding occurs every three to four hours.2
Dietary modifications can also
be useful for managing UI. Patients should avoid certain foods known to
irritate the bladder. These include carbonated or caffeinated drinks, spicy
foods, citrus fruits and juices, artificial sweeteners, and diuretics.
However, avoiding fluid is not advised, as this may worsen symptoms by
irritating the bladder.
Functional incontinence should
be managed by using environmental manipulations, scheduled toileting, prompted
voiding (e.g., asking the patient "Do you want to use the toilet?"), toilet
substitutes (e.g., portable commode), absorbent pads and undergarments, and
attention to skin care (e.g., cleansing and drying thoroughly).3
Absorbent products may not only provide overnight protection but also allow
residents to resume social activities.17
In the nursing facility
environment, easing restriction on movement while monitoring patient safety
may be all the intervention necessary to improve symptoms of UI in some
patients.22 For other patients, the use of pessaries, intermittent
catheters, or chronic indwelling catheters may be necessary. On June 28, 2005,
the Centers for Medicare and Medicaid Services issued interpretive guidelines
for the use of indwelling catheters in the treatment of UI. The guidelines
redefined UI as any wetness on the skin.25 The new guidance for
nursing homes is labeled Tag F315 and contains interpretive guidelines, a new
investigative protocol, and compliance and severity guidance.25
Only after other treatments
have been tried should surgical intervention (e.g., sling procedure or bladder
neck suspension) be recommended to alleviate UI.3
Pharmacologic Intervention
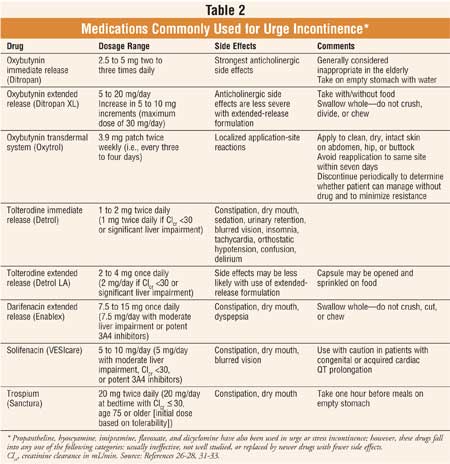
Anticholinergic Agents:
Anticholinergic agents (Table 2) are first-line pharmacotherapy for
urge incontinence, with recommended titration to tolerability and efficacy.
They are associated with adverse reactions (e.g., sedation, constipation, dry
mouth, blurred vision, tachycardia, confusion, delirium, an increased risk of
heat prostration) and should be used with caution in the elderly when benefit
outweighs risk.26 These agents should also be used with caution in
patients with urinary obstruction, angle-closure glaucoma (treated),
hyperthyroidism, reflux esophagitis, hiatal hernia, heart disease,
hypertension, renal or hepatic disease, prostatic hyperplasia, autonomic
neuropathy, ulcerative colitis, or intestinal atony.
Alpha-Adrenergic
Agonists:
Alpha-adrenergic agonists (e.g., pseudoephedrine) are used for stress
incontinence, often in combination with estrogen.15 Although well
tolerated, they may precipitate anxiety, agitation, hypertension, and cardiac
arrhythmias and should be used with caution in patients with hyperthyroidism,
angina, hypertension, or cardiac arrhythmias.18,22
Duloxetine: Duloxetine increases
urinary sphincter striated muscle tone. While experience with this agent is
limited, it appears to be effective for outlet incompetence in stress
incontinence.27
Alpha-Adrenergic
Antagonists:
Alpha-adrenergic antagonists (e.g., prazosin 0.5 to 2 mg twice daily,
doxazosin 1 to 8 mg once daily, terazosin 1 to 10 mg once daily, tamsulosin
0.4 to 0.8 mg once daily) are used in conjunction with nonpharmacologic
treatments, catheterization, and surgery for patients with overflow
incontinence.6 Bedtime administration is recommended to minimize
the risk of orthostatic hypotension associated with these agents.
Estrogen:
Studies have shown that oral estrogen in hormone replacement dosages has no
effect on stress incontinence episodes in hypoestrogenemic incontinent women.
15 In combination with an alpha-agonist, however, estrogen appears to be
effective for stress incontinence.15 Topical estrogen, applied
chronically or intermittently (i.e., one- to two-month course), is used to
treat urge incontinence or irritative voiding symptoms in women with atrophic
vaginitis and urethritis.15 Therapy usually consists of 0.5 to 1 g
of vaginal cream applied nightly for one to two months and then two to three
times per week, thereafter. Several months of therapy is usually required to
elicit therapeutic benefit.15 Estrogen delivered via a vaginal ring
(inserted every three months), vaginal tablet (inserted two times per week),
or transdermal system (e.g., a patch applied two times per week) are also
available; however, use of these treatments is generally not preferred in
patients with only local symptoms.28 These agents should be used
for the shortest duration possible.28 In patients with an intact
uterus who are using estrogen, progestin is recommended for 10 to 14 days
every four weeks.

Tailored Therapy:
Therapeutic interventions for mixed incontinence are focused on the most
troublesome symptoms. Treatment for functional incontinence concentrates on
improving functional status by discontinuing medications causing UI, treating
comorbid medical conditions, and reducing environmental restrictions. If these
measures fail, anticholinergics may be effective. Even in patients with severe
dementia, bladder training and medications have been shown to improve
incontinence.13
Botulinum-A Toxin:
Studies are reporting the use of botulinum-A toxin injected into the detrusor
muscle as a possible treatment option for patients with severe overactive
bladder (e.g., traumatic spinal cord injury) resistant to maximal doses of
anticholinergic agents and all conventional treatments.29,30
Conclusion
While UI is common
in women, it can be treated and controlled. Inadequate recognition and
management of UI can have a significant impact on a patient's quality of life
and cost of care. Appropriate treatment can assist with the avoidance of
complications and consequences including depression, pressure ulcers, falls,
and fractures. Additionally, pharmacologic and nonpharmacologic interventions
can help avoid functional dependence associated with UI. The pharmacist's
expertise proves a valuable addition to the team approach of decreasing cost
of care while increasing quality of life for patients with UI. Pharmacists can
help rule out medication-related causes of UI, recommend appropriate
medication therapy, and help patients avoid adverse drug reactions.
REFERENCES
1. Dugan E, Cohen
SJ, Bland DR, et al. The association of depressive symptoms and urinary
incontinence among older adults. J Am Geriatr Soc. 2000;48:413-416.
2. Radcliffe-Branch D, Tannenbaum C. A review of older women's health
priorities. Geriatrics Aging. 2006;9:124-128.
3. Rawlins S, Tillmanns AK. Menopause and current management. In: Youngkin EQ,
Sawin KJ, Kissinger JF, et al. Pharmacotherapeutics: A Primary Care
Clinical Guide. 2nd ed. Upper Saddle River, NJ: Pearson Prentice Hall;
2005:281.
4. Johnson TM 2nd, Busby-Whitehead J. Diagnostic assessment of geriatric
urinary incontinence. Am J Med Sci. 1997;314:250-256.
5. Levenson S. A tool for managing urinary incontinence. Caring for the Ages
. 2006;July:18-19.
6. Beers MH, Berkow R. The Merck Manual of Geriatrics. 3rd ed.
Whitehouse Station, NJ; Merck & Co. 2000: 965-980.
7. National Kidney and Urologic Diseases Advisory Board. Barriers to
Rehabilitation of Persons with End-stage Renal Disease. Workshop Summary
Report. March 7-9, 1994; Bethesda, MD.
8. Ouslander JG, Shih YT, Malone-Lee J, Luber K. Overactive bladder: special
considerations in the geriatric population. Am J Manag Care.
2000;6:S599-S606.
9. Thom DH, Haan MN, Van Den Eeden SK. Medically recognized urinary
incontinence and risks of hospitalization, nursing home admission and
mortality. Age Ageing.1997;26:367-374.
10. Nuotio M, Tammela TL, Luukkaala T, Jylha M. Predictors of
institutionalization in an older population during a 13-year period: the
effect of urge incontinence. J Gerontol A Biol Sci Med Sci.
2003;58:756-762.
11. Vigod SM, Stewart DE. Major depression in female urinary incontinence.
Psychosomatics. 2006;47:147-151.
12. Lawrence M, Guay DR, Benson SR, Anderson MJ. Immediate-release oxybutynin
versus tolterodine in detrusor overactivity: a population analysis.
Pharmacotherapy. 2000;20:470-475.
13. Klusch L. Understanding RAPS. Des Moines, IA: Briggs Corporation;
1998:23-29.
14. Wade WE. Managing dosage alteration needs in the elderly. Clinical Consult
Newsletter-American Society of Consultant Pharmacists Vol. 11, No. 10 October
1992.
15. Ouslander JG, Johnson II TM. Incontinence. In: Hazzard WR, Blass JP,
Halter JB, et al. Principles of Geriatric Medicine and Gerontology. 5th
ed. New York: McGraw-Hill, Inc.; 2003:1571-1586.
16. Kane RL, Ouslander JG, Abrass IB. Essentials of Clinical Geriatrics
. 4th ed. New York: McGraw-Hill, Inc.; 1999:181-230.
17. Couture JA, Valiquette L. Urinary incontinence. Ann Pharmacother.
2000;34:646-655.
18. Nasr SZ, Ouslander JG. Urinary incontinence in the elderly. Causes and
treatment options. Drugs Aging.1998;12:349-360.
19. Weinberger MW. Conservative treatment of urinary incontinence. Clin
Obstet Gynecol. 1995;38:175-188.
20. Rackley R, Kursh ED. Evaluation and medical management of female urinary
incontinence. Compr Ther. 1996;22:547-553.
21. Scientific Committee of the First International Consultation on
Incontinence. Assessment and treatment of urinary incontinence. Lancet.
2000;355:2153-2158.
22. Agency for Health Care Policy and Research. Urinary incontinence in
adults: acute and chronic management. Clinical practice guidelines number 2
(1996 update). March 1996. AHCPR Pub. No. 96-0682.
23. Burgio KL, Locher
MA, Goode PS, et al. Behavioral vs. drug treatment for urge urinary
incontinence in older women. JAMA. 1998;280:1995-2000.
24. National Institute on Aging. Urinary Incontinence. Available at:
www.niapublications.org/ agepages/urinary.asp. Accessed August 2, 2006.
25. Department of Health & Human Services. Centers for Medicare & Medicaid
Services. CMS Manual System. Pub. 100-07 State Operations Provider
Certification. Transmittal 8. June 28, 2005. Available
at:www.cms.hhs.gov/transmittals/downloads/R8SOM.pdf. Accessed August 25, 2006.
26. Semla TP, Beizer JL, Higbee MD. Geriatric Dosage Handbook. 10th ed.
Cleveland: Lexi-Comp, Inc.; 2005.
27. Beers MH, Porter RS, Jones TV. The Merck Manual of Diagnosis and Therapy
. 18th ed. Whitehouse Station, NJ: Merck Research Laboratories; 2006:1951-1960.
28. My Epocrates Version 8.00. Available at: www.epocrates.com. Accessed
August 23, 2006.
29. Schmid DM, Sauermann P, Werner M, et al. Experience with 100 cases treated
with botulinum-A toxin injections in the detrusor muscle for idiopathic
overactive bladder syndrome refractory to anticholinergics. J Urol.
2006;176:177-185.
30. Patki PS, Hamid R, Arumugam K, et al. Botulinum toxin-type A in the
treatment of drug-resistant neurogenic detrusor overactivity secondary to
traumatic spinal cord injury. BJU Int. 2006;98:77-82.
31. Cafiero AC, Rosenberger M, Hajjar ER. Treating urge incontinence: the role
of the new pharmacologic agents. Assisted Living Consult. 2006;2:20-23,
30.
32. Urinary Incontinence. Table 6: Potential Medication Interventions by Type
of Incontinence. American Medical Directors Association Web site. Available
at: www.cpgnews.org/UI/images/table6.jpg. Accessed August 2, 2006.
33. DeMaagd G, Geibig J. An Overview of Overactive Bladder and Its
Pharmacological Management with a Focus on Anticholinergic Drugs. P&T.
2006:462-474.
To comment on this article, contact
[email protected].