WHY YOU DON'T WANT HOMONYMOUS HEMIANOPSIA AND WHAT YOU CAN DO FOR IT
By Charles Saccarelli, ABO-AC
Release Date: June 1, 2018
Expiration Date: June 22, 2023
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Learn how patients acquire homonymous hemianopsia.
- Know what vision is like for patients with homonymous hemianopsia.
- Understand the challenges faced by a patient with homonymous hemianopsia.
Credit Statement:
This course is approved for one (1) hour of CE credit by the American Board of Opticianry (ABO). Technical Level III Course STWJHI692-3
 Homonymous Hemianopsia (HH) is extremely difficult to pronounce. It's even harder to live with. And to add to the confusion, hemianopsia can also be spelled as hemianopia.
Homonymous Hemianopsia (HH) is extremely difficult to pronounce. It's even harder to live with. And to add to the confusion, hemianopsia can also be spelled as hemianopia.
If you fancy Latin, the name tells you exactly what the condition is: Homonymous (same side) hemi (half) anopsia (blindness). So what is same side half blindness like? Many patients describe it to their doctor as having lost vision in one of their eyes. But in reality, the HH patient has a condition much more debilitating than losing vision in one eye.
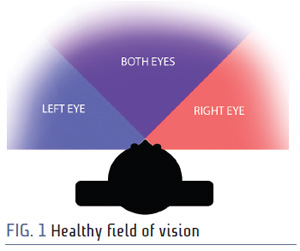
A patient with a healthy visual field has about 180 degrees of horizontal visual field. Each eye has roughly 90 degrees to the temporal side toward the ear and about 60 degrees on the nasal side toward the nose. An image of a healthy visual field is shown in Fig. 1.
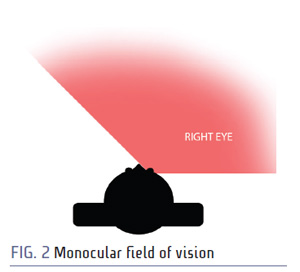 A patient with sight in only one eye has about 150 degrees of horizontal visual field (Fig. 2). The good eye has about 90 degrees visual field to the temporal side toward the ear and roughly 60 degrees on the nasal side toward the nose. So by losing sight in one eye, the patient is only losing 30 degrees or 17 percent of their horizontal visual field. There are other drawbacks to losing vision in one eye, but since this article is about homonymous hemianopsia, we're not going to talk about that. We'll stick to the visual field.
A patient with sight in only one eye has about 150 degrees of horizontal visual field (Fig. 2). The good eye has about 90 degrees visual field to the temporal side toward the ear and roughly 60 degrees on the nasal side toward the nose. So by losing sight in one eye, the patient is only losing 30 degrees or 17 percent of their horizontal visual field. There are other drawbacks to losing vision in one eye, but since this article is about homonymous hemianopsia, we're not going to talk about that. We'll stick to the visual field.
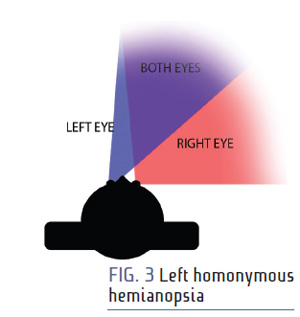 A patient with homonymous hemianopsia only has about 90 degrees of horizontal visual field. Homonymous hemianopsia can affect either side of the vision. If the patient has left homonymous hemianopsia as shown in Fig. 3, their left eye only has 60 degrees to the nasal side toward the nose, and their right eye has 90 degrees to the temporal side toward the ear. If they have right hemianopsia, their right eye only has 60 degrees to the nasal side toward the nose, and their left side has 90 degrees to the temporal side toward the ear. So by losing half their sight on the same side in each eye, they lose 90 degrees or 50 percent of their horizontal visual field. An image of a homonymous hemianopsia visual field is shown in Fig. 3.
A patient with homonymous hemianopsia only has about 90 degrees of horizontal visual field. Homonymous hemianopsia can affect either side of the vision. If the patient has left homonymous hemianopsia as shown in Fig. 3, their left eye only has 60 degrees to the nasal side toward the nose, and their right eye has 90 degrees to the temporal side toward the ear. If they have right hemianopsia, their right eye only has 60 degrees to the nasal side toward the nose, and their left side has 90 degrees to the temporal side toward the ear. So by losing half their sight on the same side in each eye, they lose 90 degrees or 50 percent of their horizontal visual field. An image of a homonymous hemianopsia visual field is shown in Fig. 3.
You may be saying to yourself: "Ain't that the darndest thing I ever did see! How does somebody get that homonyyyyy... HH?" Well, you're reading the right article. Let's take a quick trip back to grade school science class. The left side of the brain controls the right side of the body. The right side of the brain controls the left side of the body. Based on that logic, the right side of the brain would control the left eye, and the left side of the brain would control the right eye, right? Nope. That would have been too simple. Instead, our vision is split vertically into two hemifields, and the right side of the brain receives information from the left hemifield, and the left side of the brain receives information from the right hemifield.
We're not going to get too crazy on anatomy, but it's important to know what happens inside the brain that leads to a patient's homonymous hemianopsia. The figure below shows the very basic construction of the path an image takes to reach the brain from the retina.
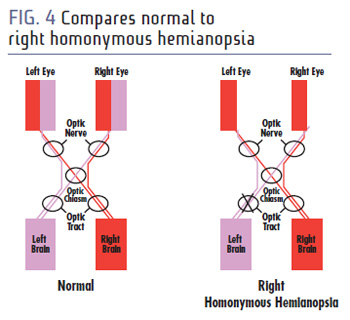 If trauma occurs to the optic nerve, a patient ends up blind in one eye. If trauma occurs to the optic tract, a patient ends up with homonymous hemianopsia (Fig. 4).
If trauma occurs to the optic nerve, a patient ends up blind in one eye. If trauma occurs to the optic tract, a patient ends up with homonymous hemianopsia (Fig. 4).
What can cause damage to the optic tract? A 2006 study of 904 homonymous hemianopsia patients found that 69.6 percent of HH cases were due to stroke, 13.6 percent were caused by trauma, 11.3 percent caused by a tumor, and 2.4 percent were due to surgery. On the bright side, another study showed that more than 50 percent of homonymous hemianopsia cases spontaneously resolve in the first six months, with the majority of those happening in the first month. So for many, homonymous hemianopsia is only a temporary condition. But for nearly half of the patients acquiring homonymous hemianopsia, it's something they will have for the rest of their lives.
So now that we've covered what homonymous hemianopsia is like from the outside, let's put the patient's shoes on for a little bit, and consider what it's like to have homonymous hemianopsia.
Are you familiar with the physiological blind spot you have in your vision—the spot where the optic nerve meets the retina? It's a spot in your vision where you are completely blind. But you're not consciously aware of this blind spot until you perform some sort of exercise to make you aware of it. Here's a common exercise. Cover or close your left eye, and look at the plus sign with your right. Move your eye in, focusing on the plus sign. When your nose is somewhere between 8 and 14 inches from the plus sign, the black dot will disappear. Alternatively, you could cover or close your right eye, and look at the dot with your left, and make the plus sign disappear. It's like magic. But it's not magic. It's your physiological blind spot. If you're viewing this on a mobile device, you may need to move in even closer than 8 inches.
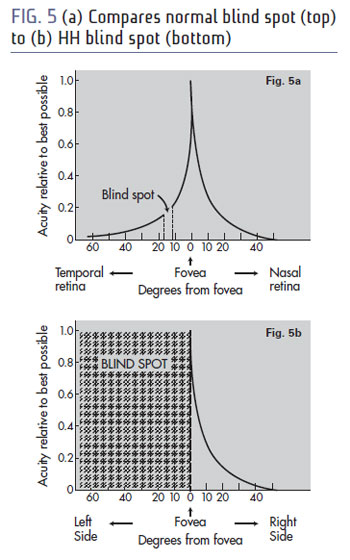 That's kind of what it's like to have homonymous hemianopsia, except a million times worse. Instead of a little blind spot, half of your vision is like that. Often times, field loss conditions are depicted with black. Black would be much easier for a patient to contend with, because they would be constantly aware of it. But instead of black, they see nothing in their blind field. And nothing is extremely difficult to simulate. But here's a try. Fig. 5a shows the depiction of a left eye with a notch of blindness for the physiological blind spot. Fig. 5b shows the blind spot for homonymous hemianopsia.
That's kind of what it's like to have homonymous hemianopsia, except a million times worse. Instead of a little blind spot, half of your vision is like that. Often times, field loss conditions are depicted with black. Black would be much easier for a patient to contend with, because they would be constantly aware of it. But instead of black, they see nothing in their blind field. And nothing is extremely difficult to simulate. But here's a try. Fig. 5a shows the depiction of a left eye with a notch of blindness for the physiological blind spot. Fig. 5b shows the blind spot for homonymous hemianopsia.
VISUAL ACUITY VS. VISUAL FIELD
Our brain has a very efficient way of processing the world around us. Picture an HDTV. Every spot on the HDTV is 100 percent resolution all the time. Our eyes don't work that way. Our eyes use maximum resolution (acuity) only in central, or foveal, vision. Our eyes then use low resolution in other areas as a cue to tell us where to look next. The chart on the left above also shows how little of our visual field is capable of maximum resolution. We only have a few degrees of vision where we're capable of our best visual acuity. Many patients with hemianopsia have perfect visual acuity. But they are missing a substantial chunk of their visual field.
WHAT MAKES HEMIANOPSIA SO BAD?
It is often said that peripheral vision tells us where things are, and central vision tells us what things are. As you move outside of central vision, your visual acuity degrades very rapidly. Your peripheral vision provides you with spatial awareness. So when a patient acquires homonymous hemianopsia, most of what they lose is spatial awareness. They see everything on one side of their body, and nothing on the other side. It's hard to imagine what that's like. To simulate hemianopsia for someone curious, you can create gaze-contingent homonymous hemianopsia with some opaque tape. Bisect each pupil vertically with the tape as shown in the figure below. The reason we call this a gaze-contingent hemianopsia is it's the only hemianopsia when you're looking straight ahead. If you moved your eyes away from the tape, you would be able to escape the hemianopsia. If you move your eyes into the tape, you can become completely blind. Patients with real hemianopsia do not have the luxury of escaping it by looking around the tape. Walking around for a little bit with this gaze-contingent hemianopsia will give a basic idea of the impairment faced by a patient with HH.
EFFECTS OF VISUAL FIELD LOSS
When working in vision rehabilitation, practitioners often give their patients and the patient's caregivers a quality of life survey to see what aspects of the condition are most devastating to them. This allows the practitioner to work with the patient directly on their concerns. For instance, if a patient loves playing cards, the practitioner can optimize the patient's care plan with exercises and devices that promote playing cards. If a patient doesn't like playing cards but loves watching TV, the practitioner would take a different approach to the patient's care. The top three concerns of most patients with homonymous hemianopsia are driving, reading and mobility.
DRIVING
Despite driving being most patients' number one goal, most patients with hemianopsia are unable to drive. Whether or not the patient is capable of driving, or has the potential to be a good driver with hemianopsia, state driving laws often dictate the legality of driving through visual field requirements. Here's a story told by Mark, a hemianopsia who was still driving.
"Giving up driving was the most difficult thing that I had to deal with. I spent months and months calling doctors and different agencies. I was looking for somebody to say, 'Yes, of course, you can drive with that vision,' but nobody would say that. And so I went ahead and drove anyway because I had a valid driver's license for five years. I'll tell you exactly what happened. It was an interesting and a scary story. I'm driving a gigantic Cadillac, a '73 Cadillac. It's huge. And I'm driving down a hill. I have a green light so I can make a turn. But the walk sign was coming the other way. So I came down a hill, and I started to make my turn, and a college student was crossing the street... a girl... just as I made the turn, and the first time I saw her was when her head went down when the front of my car hit her. And I hit my brakes. She popped up. She was fine. And I never drove again. It was just that situation that you know... could happen. The vision was missing where I really, really needed it to see her. So anyway, that was the last time I drove."
There are some states, such as New Jersey, with no visual field requirements to obtain a driver's license. There are other states with very stringent field requirements, such as New York, which requires 140 degrees of visual field but does not explicitly require doctors to report visual field loss. In Pennsylvania, a doctor has an obligation to report any patient with less than 120 degrees of visual field so their license can be recalled. In California, a patient with hemianopsia must re-pass a driving test to prove they are roadworthy with their condition. Laws vary greatly state by state. But no matter what the law is, it's important to consider the potential implications of driving with hemianopsia.
READING
In English, reading is done from left to right. Reading presents major difficulties for hemianopsia patients. Patients with left-side field loss tend to have difficulty finding the beginning of the next line of text, so they frequently get lost when transitioning from line to line. Hemianopes with right side field loss have a very difficult time because it's hard to find the end of words, so the patient constantly finds themselves re-reading words and sentences. For instance, the word "basement" might just be read as "base" and confuse the reader, causing them to start the sentence over. Reading speed is decreased significantly for all patients with hemianopsia.
MOBILITY
Difficulties in mobility are the other commonly reported issue faced by patients with hemianopsia. The lack of awareness on the blind side can cause collisions with unexpected obstacles, but mostly causes collisions with other pedestrians. This lack of awareness is most apparent to the hemianopsia patient when they are in an environment where pedestrian traffic has no specific direction, such as a shopping mall, a grocery store or an airport terminal. To the rest of the world, hemianopsia is an invisible condition. When someone is wearing a cast or carrying a cane, the rest of the world recognizes the disability and accommodates. Because hemianopsia is not visible to the outside world, the hemianopsia patient will be viewed as clumsy, oblivious or just plain rude when they collide with pedestrians. Oftentimes this leads to a psychological discomfort in going to public places.
WHY AM I READING ABOUT THIS?
"I'm an optician! What am I going to do with this information?" There is currently no surgery or pill for helping a patient with hemianopsia. That leaves practitioners with just a couple of options—training, therapy and/or eyeglasses. Do you know anyone who knows about eyeglasses? Because they'll be essential in fitting this hemianopsia patient with the various types of glasses available for hemianopsia.
Strokes are a very common condition, and a good optician has the potential to be a very important part of the hemianopsia patient's care team. Your knowledge of eyeglass availability can be invaluable to the team tasked with helping the patient not only live but thrive with homonymous hemianopsia.
GLASSES FOR HEMIANOPSIA
Most of the eyeglass designs for hemianopsia are not scientifically proven to be effective. There's a reason for this. Establishing actual scientific proof is a high bar. The gold standard for scientific proof in a medical study is a double-blind study. In a double-blind study, the practitioner doesn't know what the patient is getting, and the patient doesn't know what the patient is getting. This eliminates the possibility of the practitioner or patient bias entering into the study. If you're doing a study on pills, that's pretty easy to do. Everybody takes a white pill, and nobody knows what the white pill was until the end when the scientists are crunching the numbers to measure the results. The placebo (control) and the actual medicine (intervention) look exactly the same. When scientific studies are published, their results are published with a calculated likelihood of probability. Oftentimes, to be published, there needs to have at least a 99.5 percent chance of being accurate.
On the other end of the scientific spectrum is anecdotal evidence. The following statements are some examples of anecdotal evidence:
- But my uncle smoked a pack of cigarettes a day and lived to be 100!
- I rubbed liquefied eye of newt into my skin for 12 weeks, and the rash went away! That stuff is great!
If anecdotal evidence is collected from a large enough source—for instance, if you asked 10,000 people the ages of which their smoking uncles lived, it may possibly have some scientific merit. But it's still highly prone to bias, so anecdotal evidence should be treated with caution.
My personal favorite regarding anecdotal evidence was a conversation I've had with multiple doctors regarding a treatment that has a highly probable scientifically proven 74 percent efficacy:
Doctor: "I tried it. It doesn't work."
Charlie: "Really? Our results showed about 3 in 4 success. How many patients did you try it on to determine that?"
Doctor: "One."
I have a feeling these doctors would have scoffed at hearing the 100-year-old smoking uncle story from a patient and not even blinked at the irony.
Most glasses for hemianopsia contain prism in one form or another. It's advisable to get a patient's objective feedback through the use of Fresnel press-on prisms.
The lens design recommended by the doctor can be worn for a few weeks for the patient to get the feel for it, and then you can explore with the patient the possibility of getting a permanent eyeglass solution for their condition. We'll outline the various possible lens designs a practitioner may request for homonymous hemianopsia. We're not going to go over the potential physiological benefits and drawbacks of each lens right now. We'll do that in a future CE.
 YOKED PRISMS
YOKED PRISMS
Yoked prisms (Fig. 6) are the only solution in which you can possibly skip the Fresnel presson prism. In addition to the lens being more affordable than the other designs we'll be covering, the patient has an extremely low likelihood of experiencing adverse effects from yoked prism. A yoked prism is usually prescribed with the prism base in the direction of the field loss. Optically, this strategy will shift the patient's visual field in the direction of the field loss at all positions of gaze.
 YOKED SECTOR PRISMS
YOKED SECTOR PRISMS
Yoked sector prisms (Fig. 7) may also be called bilateral sector prisms. They are typically placed a few millimeters into the blind field. The optical effect of the lens is dependent on the patient's position of gaze. At primary gaze, when the patient is looking straight ahead, there is no optical effect. When a patient's gaze moves into the prisms, the visual field shifts toward the direction of the field loss.
 UNILATERAL SECTOR PRISMS OR BUTTON PRISMS
UNILATERAL SECTOR PRISMS OR BUTTON PRISMS
Unilateral sector prisms (Fig. 8) and button prisms go by many different trademarks, but all have the same basic optical principles. At primary gaze, there is no optical effect. At a gaze into the prism, the visual field of the eye with the temporal defect's visual field shifts in the direction of the field loss.
 PERIPHERAL PRISMS
PERIPHERAL PRISMS
Peripheral prisms (Fig. 9) use a couple of unique optical principles called vision multiplexing and visual confusion. Rather than looking through the prisms, the patient looks between the prisms. At primary gaze, the visual field of the eye with the nasal defect has no optical effect. Images from the blind side are shifted into the seeing field on the eye with the temporal defect.
CONCLUSION
Homonymous hemianopsia is a devastating condition that affects a lot of people. The patient's visual field is cut in half right down the middle. It affects their ability to drive, read and ambulate. Through the placement of Fresnel prisms under the direction of a doctor and through the manufacture of highly specialized lenses, an optician has the opportunity to be an important part of the hemianopsia patient's care team. We'll cover prism correction for this condition in more detail in a future CE course.



