By Barry Santini
No aspect of a brick-and-mortar optical communicates its commitment to quality better than the pride in stating “Accurate eyewear made here.” Clearly this makes sense, as two of the top reasons that consumers give for leaving their present optical is “My glasses were made wrong,” and “I no longer trust them.”
So part of Job #1 is to avoid incorrectly made eyewear arriving at the dispensing desk. To this end, eyecare professionals must be eternally vigilant to track the common errors when making prescription eyeglasses—a custom made precision optical product that masquerades today as a commodity made in an assembly-line environment.
But even while adherence to best practices to reduce error in the eyewear dispensed does not guarantee wearer satisfaction, continued tracking of error remains fundamental to every stage of the eyewear fabrication process. From patient intake to dispensing outtake, maintaining fidelity to the Rx and the order specifications is the goal of laboratory processing. Hearing wearers exclaim, “These are perfect!” will always be preferable to saying, “You’ll get used to it.” Let’s look at the areas of potential error that should be tracked when fabricating eyewear.
WALKING A TRICKY TIGHTROPE
As I explained in my 20/20 article “Do Eyewear Standards Still Matter in an Online Age?” (April 2017), when establishing acceptable tolerances for error, the first ophthalmic lens ANSI standard attempted to define what levels of precision and accuracy were theoretically possible to achieve—without regard to the costs of doing so or the actual benefit to the eyeglass consumer. Subsequent revisions of the standards became more globally informed and began to weigh the cost-benefit ratio of high precision more realistically. This resulted, for some parties, in an unacceptable loosening of the standards, best illustrated by the oft-heard phrase “ANSI is for amateurs.”
But this low tolerance for error approach has a dark side: Creation of a slavish or fetish-like fabrication culture, devoted to achieving exceptionally low tolerances that deliver no tangible benefit for the ultimate beneficiary—the wearer. That being said, the most important thing for dispensers to know is when strict adherence to tolerances matters and when it does not. This is the tricky tightrope all ECPs must walk. Yet it ultimately leads to high confidence in deciding which areas matter most for any specific wearer.
Tracking error in eyewear really begins by understanding how to avoid it in the first place. The best place to begin is at the dispensing desk, when the optician reviews the changes, if any, present in the patient’s newest Rx.fitting and demonstration tools.
THE RX: THE PLUS AND MINUS
The goal of tracking error is to avoid it in the first place. Let’s begin with the Rx:
- Transpose every prescription to minus cylinder form—Although lab management systems (LMS) can auto-transpose between the two Rx conventions, the review process for both order entry and subsequent verification of both uncut lenses and finished eyewear—especially with those having position of wear (POW) compensations—is always done in minus cylinder form. Even if you individually are facile in Rx transposition, other coworkers or staff who must review or answer questions regarding the Rx or prescription history may not be.
- Correlate the Rx change to the degree of complaint—Every ECP should ensure that both they and the patient have a clear understanding of the degree of visual impact forecasted by the new prescription. Often, simple misunderstandings—such as which lens or portion of the Rx is changed more than another—should be understood by both parties right from the get-go. This will ensure greater confidence in the final prescription and facilitate greater patient willingness to consider better lens technology instead of trying to stem losses if they lack confidence in the Rx outcome. Buying eyeglasses remains enough of a trial for the public without having to start out on the wrong foot.
- Don’t be afraid to say no—Especially if your office routinely fills outside Rxs—as I do—do not be afraid to advise a buyer against purchasing new lenses if there’s a clear disconnect between your understanding of what the new eyewear will accomplish and theirs. In the long run, only by being seen as a trusted source of advice and counsel can a brick-and-mortar optical survive the ongoing commoditization of the eyewear industry. There will always be competitors who have products you don’t at prices you can’t match. But only the B&M channel has the potential to enjoy a bond of high trust between buyer and seller that makes buyers say “I wouldn’t think of going anywhere else.”

ORDER IN THE OPTICAL
Once the order for eyewear is written, it’s onward to the ordering portal for your chosen lab partners. Before sitting down at the computer to place the order, you should review the following areas:
- Understand your order—I know that when I get slammed out front, I tend to adopt a type of shorthand for writing down the essential of PD, height, POW values and lens information. As I’ve aged, I find that I can’t rely on my formally robust memory to save me if I forget to write things down or can’t decipher my handwriting. Calling upon discipline garnered from years of being a classical music instrumentalist, I have trained myself to write the essentials in a way I can teach others to understand easily. You should too. Whether your passion has been cooking, sports, academia, crafts, hobbies or music, try to transfer the discipline learned from any accomplished pursuit to writing eyewear orders that will ensure the eyewear is made as intended.
- Double check all measurements—From pupillary distance to pupil height, compare and contrast your new measurements to those previous values on file or to those in their present eyewear. For the PD, your monocular values can and will vary over time, but the binocular PD sum for an adult should not vary more than a millimeter. If they do, that’s a flag to double check. As for pupil heights, they will obviously vary from frame to frame. But a double check is to calculate how many millimeters above the frame’s vertical midpoint the new pupil height falls. What you’ll discover is how often this value is consistent between frames of similar B dimensions. And while frame wrap angle varies from frame to frame, pantoscopic tilt and vertex distance are more often similar between frames of like wrap angles. Good to know, especially if you forgot to take these measurements when you’re slammed on a Saturday—post pandemic, of course.
- Take vertex distances—Although vertex distance has been long associated with lens power compensation, in today’s more advanced free form lenses, vertex distance—along with panto and wrap—is used by the lab’s lens design system (LDS) to ensure global correction of the entire lens surface and not just the axial area in front of the eye. Keep in mind, however, that the majority of LDS do not compensate lens power for differences between refracted vertex and fitted vertex. Most of the time, the dispenser must perform this power compensation before entering the Rx values. This is also good to know.
- Scan the frame—The gold standard for obtaining the best from personalized free form lenses is uploading a trace of the individual frame chosen. Using the actual lens shape—rather than using simple frame dimensions or choosing a generic shape—allows the most precise Rx and thickness optimization possible. But many offices lack the capability to upload individual frame shape information. An alternative is to enter the frame name, brand and boxed-frame measurements. Many lab management systems can use this information to access an extensive archived library of frame shape data—including the equivalent eye wire tracing—as an acceptable substitute for an uploaded tracing. As an added bonus, groove and drill point lens thickness can be even better optimized using individual drill point data. Where possible, be sure to enter the frame manufacturer or even distributor in order to reduce confusion between similarly named frame styles between companies. With some lens manufacturers, such as Carl Zeiss, now moving to a watermarked brand logo even on uncut lenses—the only way to ensure optimal placement is through an uploaded tracing or frame-specific information.
- Take a bird’s eye view—After entering your order on the lab’s portal, it is imperative to pause and review all that you have entered. I find that the most easily avoidable errors are the ones easiest to catch by taking the time to review this. I also find it useful to narrate the entire order as if it was an unfolding story.
- Is the patient’s name spelled correctly?
- Is the order number correct—especially on multiple orders for the same client?
- Read the Rx.
- Check the PDs and fitting heights.
- Check lens design, material, color and treatments.
- Check position of wear measurements, if any.
- Check requested base curve, if any.
- Check frame type entered, i.e., metal/zyl, grooved, rimless, sport, etc.
- Check frame name, brand and boxed measurements.
To this end, I wish more lens ordering portals would reformat the order of the entry fields to more closely follow how eyeglass orders are written in the real world. For example, it would be nice to enter the Rx ADD power right after entering the distance Rx—and not after choosing lens design and material. If all the lens portals tried to be more human-factor optimized and consider how dispensers typically think about and enter job information as opposed to how lens systems process the order information, I believe there would be a lot less avoidable errors in order entry.

THE FINAL APPROACH
Regardless of whether you fabricate your office’s eyewear in house or receive completed jobs from your labs, keep in mind how the nature of humans often colors what’s termed acceptable to pass along to the customer:
- People will always forgive their own mistakes more than the mistakes of others. So take it easy on your lab.
- People will pass errors on the third redo that they wouldn’t have passed on the first or second.
- People will transfer blame for job delays and errors onto others—especially their lab—before they will accept ownership themselves.
All I have to add to the above is two words:
Mea culpa—though I am working daily on overcoming these tendencies.
DON’T BE LAZY
The best advice for tracking errors is to remain ever vigilant. But this type of commitment takes extraordinary discipline—the type not unfamiliar to the accomplished musician, athlete or university scholar. One has to earnestly resist the natural tendency to become lazy. So if you’re more interested in having a beer than understanding the boxing system, perhaps it’s time to change careers. Remember, no amount of ever-finer error parsing will guarantee wearer satisfaction. Rather, the eyecare professional of the 21st century is all about walking the tightrope of deciding what’s acceptable for a particular patient. And no online entity will ever have access to the amount of personal information a brick-and-mortar office does when ensuring that the things that matter are properly matched to the individual wearer.
THE PRISM DILEMMA
What is it about the presence of prism in a prescription that makes the hair of opticians stand on end? Is it because it’s encountered with such low frequency? Or is it that most only think of prism when its written in the prescription?
More than any other lens parameter, prism is—to use a term borrowed from IOT’s Tina Lahti’s—squishy. What Lahti means is that the bump stops that define what our vision will tolerate are ill defined. And that is both the good news and the bad news. When you review eyeglass centration, there is only one cardinal point—the prism reference point (PRP)—at which prism or its absence can be clearly verified. The good news is how much our eyes can manage to maintain comfortable binocularity without apparent complaint. The bad news is that as the power imbalance between the eyes becomes more complicated by prescriptions of dissimilar power and/or oblique astigmatism, both patient and practitioner often don’t realize the insidious impact of imbalance until vision fatigue, dry eye, headache and other symptoms of asthenopia finally surpass an individual wearer’s threshold of comfort.
As eyecare professionals, we must guard against becoming cavalier about situations of no obvious complaint—meaning a wearer may have simply gotten used to it because human vision is squishy. The only thing ECPs need to get used to is understanding the mechanics of handling prism and reducing unwanted imbalance through proper lens design and placement.
PROPER DESIGN AND PLACEMENT FOR PRISM
Particularly in prescriptions having any amount of prism greater than a total of three diopters, every dispenser should try to prioritize selecting a design and placement where the lens’ PRP is placed directly over the pupil height. Unfortunately, wearers don’t always gaze straight ahead in their daily activities. As the eyes depresses to read, answer a cell phone call, or step off a curb on a busy street, placing the PRP at the pupil means there’s a greater likelihood that undesirable imbalance will reside in the near area of the lens. This is particularly true in progressive lenses, which is the reason why progressive PRPs are located between 4 mm and 6 mm below the fitting cross as a compromise between distance and reading priorities. Also, placing the PRP in this manner often improves the cosmetics of stronger Rxs. But therein lies the dilemma: Prioritizing cosmetics in prism prescriptions almost always works against delivering the best optics.
There are lens designs today that prioritize optimizing prismatic effects across the lens, such as the Shaw lens, Hoya iD MyStyle 2, Zeiss Individual SL, among others, that should be among your go-to lenses when handling prismatic, anisometropic or antimetropic Rxs. But if you or your lab does not know how to properly edge progressive lenses with prescribed prism, the wearer may not experience optimal overlap of the progressive corridors. Handling prescribed prism is an often overlooked source of placement error with progressive lenses.
DON’T BE A BLOCKHEAD
If you’re like me, you may have been blocking progressives with prism for years, blissfully unaware of the modifications needed to ensure proper overlap of the progressive corridor. When finishing these lenses to a frame, you must compensate the blocking center by changing the blocking point approximately 0.25 mm per prism diopter in the direction of the apex. For example:
Rx:
OD -2.00 -0.50 x 75; 3D Base Up; 2D Base In
OS -0.75 -1.00 x 105; 3D Base Down; 2D Base In
PD: 30.0/32.0; Height: Rt 22 mm; Lt 23 mm
The PD and height adjusted for blocking results in the following values:
RT: PD 30.5 mm and Height 20.25 mm
LT: PD 31.5 mm and Height 23.75 mm
The finished heights may appear incorrect, but I assure you they are not. However, this adjustment does point to the need for improved accuracy when taking PD and height measurements in prismatic progressive prescriptions.
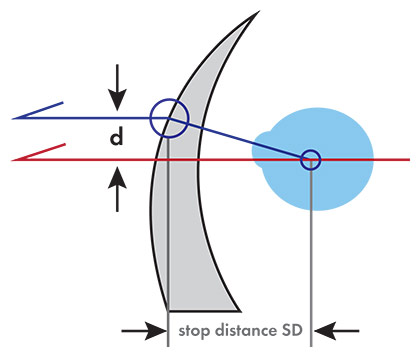
TRACKING ERROR IN WRAP RXs
When blocking lenses for edging, remember that the lens plane of the blocker assumes a zero-degree wrap angle. So a frame that possesses any degree of wrap—and most frames typically exhibit between five and seven degrees—must have a compensation made to ensure proper final centration. Wrapping a frame front changes the effective “PD” of the frame, decreasing it from the simple sum of the eye size and DBL. So lenses blocked at a 62 mm PD—in a frame wrapped to 7 degrees—will result in the finished distance between lenses narrowed to 61.54 mm. Greater amounts of wrap angle will result in greater reductions in frame PD. To compensate for this, you could either widen the “blocking” PD or adjust/narrow the DBL value. In the above example, if the actual DBL was 15 mm, you would decrease it by 0.46 mm and enter an adjusted DBL of 14.54 mm. I prefer adjusting the DBL to compensate wrap angle when blocking lenses, since this way allows staff to use the original PD. Many of today’s advanced tracer/blockers will adjust the DBL for the entered wrap angle. In any case, the most overlooked blocking situation in wrap frames occurs when the frame is a groove mount or a rimless. If these frames have a wrap angle greater than 4 degrees, you must remember to compensate the blocking point to avoid an unintentional centering or prismatic error.
—BS
Contributing editor Barry Santini, A.A.S., ABOM, is a New York State licensed optician. He is ABO certified and was awarded an ABO Master in 1994. He has been an owner of Long Island Opticians in Seaford, N.Y., from 1996 to present.













