
By Barry Santini
Compensated eyeglass lenses are an important and ever-present part of the daily optical lives. They offer the promise of evermore refinement in visual acuity by addressing the optical differences in tilt, wrap and vertex distance that exist between the lenses used in an exam and the reality of how frames fit in the real world.
Yet as recently as 20 years ago, these “position of wear considerations” weren’t really part of the daily conversation in a typical optical shop. What happened? What changed?
Certainly the scientific approach to ophthalmic optics—already more than 70 years old at the millennium—did not require wholesale reinvention. Rather, it’s more likely that the arrival of progressive lenses—and the significant challenges they posed for early wearers regarding adaptation and comfort—sparked the lens industry to address the issue of how these lenses could be made more wearer friendly. Lens designers discovered that the best way to achieve this was by incorporating custom position of wear measurements into the prescription, thereby compensating for the lack of personalization found in conventional lenses.
WHAT CHANGED?
The best place to begin is by understanding why a frame’s position of wear mattered in the optics and adaptation of a progressive lens is to embrace the concept of 20/Happy vision—a term I use to describe the careful balance between acuity, comfort and utility that is specific to each individual wearer. Without a good balance of these factors, wearer unhappiness is sure to follow. Before the desire for fashion entered the function of dispensing eyewear, frames were small, symmetrical and—more often than not—fitted on or close to center pupil with regard to the lens’ size and shape.
With the arrival of larger nonsymmetrical shaped lenses in the 1940s and ’50s, the eye had a lot more room to roam away from center. This didn’t really create much in the way of optical problems, as the steep contour of a corrected curve lens delivered acceptably sharp peripheral vision in an era when frame sizes rarely extended beyond 50 mm. But much larger frame styling entered the industry in the 1970s and ’80s. This, along with the popularity and appeal of progressive lenses, and the introduction of polycarbonate lenses negatively impacted how many wearers felt truly 20/Happy. By the mid-1990s, the compensated lens technology offered a possible remedy.
WHY COMPENSATED LENSES?
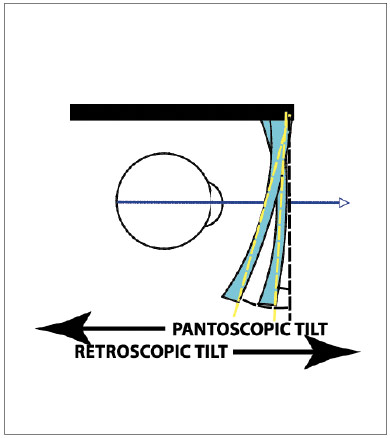
The fundamentals of refraction and vision testing—although improved by advances in technology—have not fundamentally changed in over a hundred years. Even today, in a typical exam room, small flat lenses—held in a flat plane and centered perpendicular to the eye’s distance gaze remains the standard for both objective and subjective testing of sphere, cylinder and axis. But how the actual eyeglasses fit is another story: Frames are often wrapped, tilted and spaced from the wearer’s eye according to the dictates of fashion, function, anatomy, fitting preference and the reality of gravity. The fitting differences that exist between the examination lenses and the real world fit of fashion eyeglasses became problematic when adaptation problems surfaced in the fitting of early progressive lens designs.

THE FITTING DILEMMA
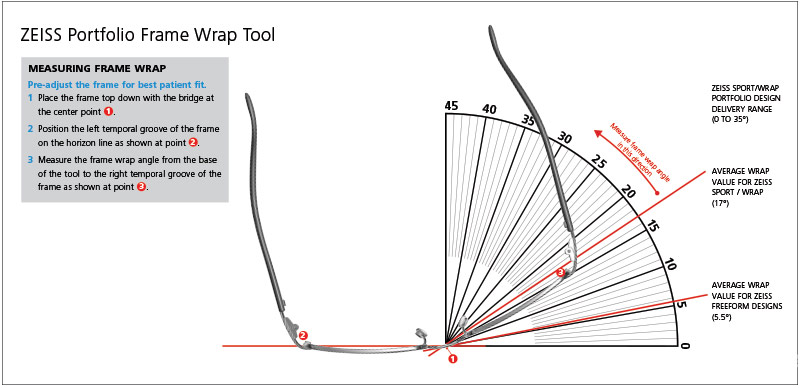
If eyeglass frames were aligned like exam lenses—flat and perpendicular to the floor—the eye would encounter unwanted variations of vertex distance and obliquity of peripheral rays as it traversed larger frame’s sizes field of view. This situation facilitates unwanted magnification changes and increased peripheral astigmatism as the eye moves beyond the primary gaze angle, a situation particularly common when reading. Although not as impactful in bifocals and trifocals, frames with zero angle and pantoscopic tilt angles inherently increase the swim and distortion experienced with progressive lenses. In the early progressive designs, lens companies recommended a fitting solution: Adjust the frame to a pantoscopic tilt of 8 to 10 degrees and a companion frame wrap angle between 5 and 7 degrees. By fitting a frame this way, you reduce variations in vertex distance and the obliquity of peripheral field rays. This reduces both magnification variances and oblique astigmatism across the wearer’s entire field of view. Both of these aberrations are undesirable in any lens, but are tolerated better in simpler lens designs and presented a particularly poor match for the less sophisticated/harder progressive designs of the 1960s and 1970s. But then as now, trying to adjust any frame to these values isn’t an easy task for a multitude of reasons. And even if this progressive-friendly frame fit was achieved, it came with a cost: It introduced unwanted power and astigmatism errors at the primary gaze point, induced by the increased pantoscopic lens tilt. Further, horizontal prismatic imbalance was induced by the increased frame wrap angle. This was the fitting dilemma that eyecare professionals encountered as they tried to move bifocal and single vision wearers into the seamless vision of progressive lenses.
LEARNING TO TRUST COMPENSATED LENSES
Troubleshooting a pair of conventional glasses can be hard enough, and a compensated set of lens values could clearly make it harder. Why? Because your being asked to accept changes in prescription that are not consistent with you daily experience. In reality though, troubleshooting compensated progressive lenses is no different than with non-compensated lenses. You simply begin at the beginning:
- Verify that the lenses are, in fact, made and fitted within ANSI tolerances to the supplied compen- sated values.
- Review both the nature and direction of change in the new prescription against the old one.
- Interview the patient to discover what visual problems areas they experienced in their previous pair and what they expected would improve with the new pair.
- Carefully record which side of the applicable tolerances for sphere, cylinder and axis both the new and previous pair were made.
Now you begin the analysis. This is one of the skillsets that clearly differentiates that novice optician from the experienced one, and it is guided by one over-arching principle: knowing when to double-down on doubt.
–BS
FREEFORM ADDRESSES THE DILEMMA
It should be clear that the values given above for pantoscopic tilt and frame wrap will provide a more optimal fitting situation—if it didn’t come with variation in magnification and unwanted or increased astigmatism error. But when freeform lens surfacing arrived in the mid-1990s, it finally became possible to address these optical negatives by using a lens surface having far more precision and sophistication than the most finely made molded or spherical surfaces in use up to that time. Combined with advances in lens tracing and real time lens design optimization, it was now possible to optimize the optics of any lens type—progressive or single vision, for individual frame’s position of wear. By the early 2000s, lens companies were trumpeting ever more sophisticated ways to compensate the optics of a tilted and wrapped eyeglass frame.
But ECPs weren’t yet ready to understand or embrace the idea that they now needed a set of compensated prescription values that were different from the doctor’s Rx. And they were reluctant to allow eyewear made this way out into the real world on the faces of their trusting clients. Catastrophic scenarios peppered the minds of eyecare professionals everywhere:
- What if they went back to their doctor and they checked the glasses and found them “wrong”?
- What if the patient didn’t see well?
- Where would you begin to troubleshoot if a patient came back dissatisfied with their new vision?
- What if the compensation was done wrong—or too much?
THE MYSTERY OF THE RX
When troubleshooting progressive complaints—especially with compensated lenses—you have to be open to considering all the suspects:
- Lens design—hard or soft.
- Corridor length—long, medium or short.
- Frame fitting differences—size, depth and position of wear.
- Material and abbe differences.
- The impact of any added or deleted lens treatments.
- The actual changes in Rx sphere, cylinder, axis and add power.
The first five should be familiar to all. But casting doubt on the last one—what the new Rx changed—has been generally frowned upon. Why is that? It’s because any carefully arrived at Rx, in reality, represents an informed, optimal and intentional balance between all factors in the mind of the prescriber for that patient. But it can also be a puzzle whose mysteries and solution you might be asked to unpack on the way to achieving 20/Happy:
- Examiner discretion: Every examiner wants only the best vision for their patients. The transformation of refractive findings into a new prescription is literally a process that is directly influenced by both their experience and desire to make the new Rx as easy to adapt to as possible. To this end, examiners may intentionally modify the final Rx from the initial refractive finding any of the following ways in order to minimize unwanted perceptual side effects:
- Reduce or eliminate small cylindrical powers.
- Cardinalize the Axis of Astigmatism (moving otherwise oblique axes closer to the cardinal directions of 90 or 180).
- Patient doubt: To be sure, no examiner intentionally issues a new prescription that they think will be problematic, although sometimes they do suspect an Rx may present an adaptation challenge for the patient. Sometimes that doubt is communicated, and sometimes it’s not. But even if that doubt is communicated, it is often conflated with the doubts felt by the patient during the heightened state of anxiety in subjective testing—especially if the process is perceived as rushed, or if they felt the examiner was too perfunctory. Feelings such as “Did I answer correctly?” or “The choices seemed rushed” can be common, and may predispose the new wearer to expect trouble with their new glasses. Bottom line: Doubt in the exam room creates doubt at the dispensing desk. This means troubleshooting eyeglass problems should always include a tempered doubt about what the prescriber’s intent was in any new Rx.
- Keeping the add power to a minimum: Again, this is not a bad approach per se. But it is important for every optician to know that the effective add power can be impacted by the choice of lens design, corridor length and frame fit. Sometimes the add power will have to be modified—either up or down—to get that patient to 20/Happy.
THE LAB’S JOB AND YOUR JOB
At this point, you should be thinking: “All this is good to know. But how does this relate to understanding and troubleshooting complaints with compensated lenses?”
Here’s how: Blindly applying equal tolerance to a target Rx value with compensated lenses, i.e., power and axis specifications, is the lab’s job—not yours.
The charge of compensated lenses, by definition, is to tweak and adjust the Rx values to compensate for the differences between the alignment of the exam room lenses and the reality of a frame’s actual position of wear. And whether you supply custom fitting values or let the lab’s lens design system (LDS) employ default fitting values, it should be clear that sometimes a combination of the various unknowns described above may result in an out-of-tolerance situation for a specific individual’s visual satisfaction. This is the very definition of 20/Happy.
COMPENSATED LENSES AND 20/HAPPY
We hear so much today about compensated lens values. They can be alternately confusing, frustrating or inspirational. The intent of compensated lenses has been said to “deliver the Rx the doctor intended.” But sometimes the intent of the Rx is not fully understood or appreciated by all parties. My best advice: Stop fetishizing and spending your or your lab’s time and money chasing tolerances more precise than what ANSI suggests. “ANSI is for amateurs” does not mean you should try to be hundredth-of-a-diopter precise. Rather, it means that just applying ANSI tolerances, as a lab does, could prevent you from advancing as an eyecare professional. Remember that at any interactive level above the lab generally has access to far more global information and data about an individual patient than a lab’s work order does. The lab’s job is defined at one or more levels of sophistication and nuance below yours. You are capable of making a far more informed judgement about what is appropriate or not appropriate for any individual patient.
Even today, ECPs continue to narrowly think of compensated lenses in terms of distance and reading powers—which completely overlooks the more important global optimizations going on across the rest of the lens surface. The worst situation is when an ECP, after having a few frustrating experiences with patients and compensated lenses, wrongly concludes that compensated lenses are nothing more than an unnecessary and expensive complication in their lives and therefore should be avoided.
KEEPING GROUNDED
While our professional field has always had one foot grounded in the world of scientific optics, the other foot remains firmly and unavoidably planted within the world of individual human sensory experience. Because ECPs are fitting appliances that impact the primary way human beings gather information about and interact with the world, the perspective that ECPs should retain about compensated lenses is that they are among the greatest advancements yet in the science of ophthalmic optics. But they also cannot be seen as the end all cure for any optical will. Once in a while, even optics will have to take a backseat in the journey to get every wearer to 20/Happy.
When Worlds Collide: Getting Back to 20/Happy
What follows is a cautionary tale, one that reveals how the Rx you’re given, together with an unusual Rx compensation and unfavorable ANSI tolerance can keep a pair of glasses from delivering 20/Happy.
History:
The patient is a 72 year old post cataract senior. They have been using +2.50 OTC readers, and apparently happily for the last year or so. Patient says they have no DV Rx after surgery and declare they see fine. But now they desire to purchase a set of brand name/authentic prescription progressive sunglasses in a wrap sport frame style. They deposit the following recent Rx on my desk:
OD +0.50 -1.00 x 90
OS +0.50 -1.00 x 90
Add OU: +3.00
Rx Analysis:
“Wow,” I think to myself. That’s a bit of distance Rx to have post-op and feel they see “fine.” But I quickly realize that the above Rx translates to a PLANO spherical equivalent-so no harm/no foul. Makes sense. But that +3.00 add does not—especially if they’ve really been “happy” with +2.50 OTCs. So I decide to second guess the add power and reduce it to +2.75—especially in view of the fact that the frame chosen is a sport style with a healthy frame wrap angle of 25.5 degrees.
Receipt and Verification of New Sunglasses
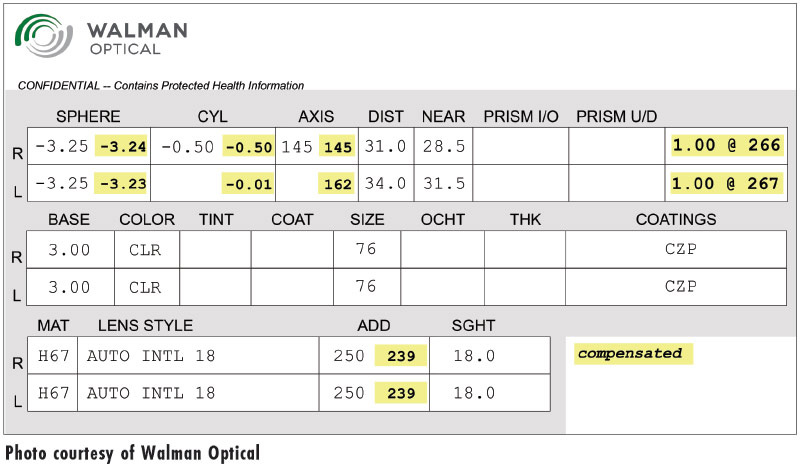
The new sunglasses arrive in 10 days, with the following compensated Rx for verification purposes:
OD +0.64 -0.96 x 86
OS +0.64 -0.97 x 93
Add OU: +2.38
The glasses, however, end up neutralizing at:
OD +0.74 -1.01 x 87
OS +0.74 -1.02 x 92
I verify the above power on both my trusted automatic Huvitz lens meter and a manual Topcon lens meter. Conclusion: Yep, they are “within” ANSI tolerance for sphere, cylinder and axis. But I don’t like where the final sphere power is falling—namely, to the “plus” side of the power tolerance. (We’ll uncover why I feel this way later in the story.)
Delivery of New Glasses
Patient comes to pick up glasses and is very excited: They had bought into the whole brand performance aspect of these authentic lenses and were looking forward to getting their glare and reading issues addressed. They put them on, test the distance and reading vision, and pronounce them “terrific.”
They return a week later, somewhat less than 20/Happy: Distance vision is slightly blurred and reading requires them to look “too far down” into the progressive to see clearly. I verify the fitting height is correct and not too high, as well as the engraved add power. I then go to my handy Rx Flippers to perform some over-glasses diagnostics. The following quickly becomes clear:
- The Distance Rx benefits from the addition of -0.25D to achieve clarity.
- The Reading Rx benefits from the addition of +0.50D to achieve clarity and comfort.
I subsequently trial frame the original distance and reading prescriptions. I find that the distance is fine when the sphere power is +0.50—but not +0.25D more. The Reading Rx alone tests out to the prescribed +3.00 add. (Sorry doc, for doubting you.)
The Glasses Are Redone
I decide to return the glasses and order the following Rx based on my experience with the flippers:
OD +0.25 -1.00 x 90
OS +0.25 -1.00 x 90
Add OU +3.25
The redone glasses arrive 10 days later with the following compensated values:
OD +0.35 -0.96 x 86
OS +0.35 -0.87 x 93
Add OU +2.86
Neutralization reveals the following found distance power values:
OD +0.54 -1.01 x 87
OS +0.55 -0.89 x 93
I decide these values are what I was targeting and call the patient in to try the redone glasses. (Note: I rarely use my lens meters to verify the received add power. For this parameter, I will take the “manufacturer's word for it,” unless there is strong reasons present to doubt the received add power values.)
Result? The patient achieved clarity for both distance and reading.
Getting to 20/Happy
Any good prescription is the result of careful objective and subjective testing, mixed with a review of the patient’s visual history, and the experience and discretion of the examiner. There is no doubt that the original Rx was a terrific Rx for overall use—but was also one that bordered on being a bit too much plus for use with a darkly tinted sunglass routinely used for outdoor distances much further than the test normal testing distance of 20 feet. When the slightly too-strong original sphere powers collided with a compensated Rx that also went to the plus side of plano and arrived with a fabricated sphere power that—although was within ANSI tolerance—moved the spherical equivalent too far to the plus side for a pair of glasses meant for extreme distance vision.
Could this redo have been avoided? Perhaps. And perhaps not. Even though the patient initially revealed that they see distance fine without glasses and read fine with +2.50 OTC readers, it’s clear there was more to their actual state of vision than their anecdotal “20/Happy” summary.
My Rx recommendations for sunglasses:
- Prescribers should ensure that an Rx meant for sunglasses Rx is never to the plus side of 20/Happy because sunglasses are not used indoors. An Rx biased to the plus side of distance clarity would be a fine overall Rx for all activities except long distance, outdoor use.
- Although compensated Rx values should fall where they are calculated, the fabricated RX should never been allowed to tolerance in the same direction as the compensated sphere values when compared to the ordered Rx.
Are these suggestions workable in the real world? Probably not. But it does make a strong case that trained opticians should be able to adjust any Rx to whatever it takes to get any pair of glasses to that visual nirvana we call 20/Happy.
–BS
For more on this topic, read Barry Santini’s RxPertise feature, “20/Happy: Independent Thinking that Redefines Eyewear Value in the Online Age” in the June 2016 issue of 20/20.
–Andrew Karp
Contributing editor Barry Santini is a New York State licensed optician and contact lens fitter with Long Island Opticians in Seaford, N.Y.













