
By Barry Santini
Today’s advanced free-form progressive lenses offer both fitter and wearer more clarity, comfort, visual utility and personalization potential than any multifocal ophthalmic lenses ever made. But many eyecare professionals still rely upon older front surface PAL designs as their go-to lens choice, despite many of these designs dating back 25 years or more.
At the beginning of the new millennium and before the full emergence of free-form technology, the race among competing lens companies was mainly centered on trying to create the best overall progressive. Although this race continues today in the top-tier lens class, these all-purpose designs are now but one part of a multi-level product offering that includes targeted applications optimized for virtually any visual task.
The challenge for the optical industry is to recognize that today’s eyewear consumers are actively seeking out more varied and better-quality products, and while still mindful of price, they are no longer passively waiting for their ECP to recommend or prescribe them based on an appraisal of need. To answer consumers’ expectations, ECPs will have to up their progressive game, which includes having a strong understanding of the increased sophistication resident in today’s free-form technology, exactly what compensating a prescription actually means and why these compensations enhance sharpness to the end wearer—even if a hundredth of a diopter precision exceeds the eye’s ability to discern. ECPs will also need to understand the evolution of progressive design, as well as where the most revolutionary progressive advances are expected to come from.
Let’s begin by challenging a few of the current assumptions in the fitting and use of glasses.
PERSONALIZED LENSES:
NEVER ASSUME
The period of progressive lens design between the introduction of Varilux 1 and the beginning of the new millennium could be characterized as a race to create a single “best” overall progressive. But this approach had limitations, because it was handicapped by the need to make assumptions about how glasses would fit. In part, this was because of the more limited technology of the day, but also because of the prevailing thinking about how glasses fit, the state of the eye’s pupil, and what consumers really wanted and were willing to pay for in their glasses:
1. Assuming the position: Before the advent of free-form technology, an ECP could not enter personalized fitting values for pantoscopic tilt, frame wrap angle and vertex distance. So lens companies would only design to a set of assumed fitting values. And the values they chose for panto, wrap and vertex were based on an average of values found in the fitting trials of the day. The problem here is that both frame style and fashion remain fickle and fluid, and this, combined with single-sized frame design and construction meant that the real world position of wear was often more than a bit removed from the fitting values the lens designer had assumed. The result was and still is reduced real world performance.
2. The public wants or needs only one pair of glasses: Although this may have been true 50 or more years ago, the arrival of name-branded frame lines and the anticipation for periodic style changes have placed eyewear squarely into the cycles of fashion. Although it has some distance to go, eyewear is well on its way to being treated with the same fashion want and appeal as apparel and shoes. Certainly plano sunglasses have moved ahead of prescription eyeglasses in this regard, with consumers routinely assembling a wardrobe of multiple pairs. The takeaway here is that consumers are beginning to fully embrace the idea of owning more than one pair, if not just for need, then ultimately for fashion. Today, cases that can handle multiple pairs are carried not just for need, but also for the freedom to indulge in a mid-day makeover. If you contrast this with the inconvenience of carrying a backpack for a mid-day change of wardrobe, eyewear wins on convenience alone by a mile. The point here is that today, multiple pairs are being approached in multiple ways.
3. The puzzle of pupil size: The pupil of the human eye is far from static, ranging in distance fixation from 2.5 to 4 mm during the day, to as much as 5 mm to 7 mm at night. At any level of ambient illumination, the pupil will construct during intermediate and near accommodation to improve depth of field. Even armed with the knowledge of a large range of pupil sizes, designers of earlier progressives could not fully implement the idea of a dynamic pupil and settled on pupil size between 3 mm and 3.5 mm. But the full impact of daily changes in pupil size is not only about light or near focus. Pupil size directly determines what cross section of the eye’s optics, from cornea to lens, is being used to focus the retinal image. Here the pupil is acting as a stop, limiting the cone size of incoming light, including that coming from the periphery. Most ECPs recognize why large pupil sizes can degrade retinal image quality but are less aware of how nuclear cataracts may impact sphere, cylinder and axis when the pupil constricts during near focus or bright light.
Older progressive designs had no choice but to use averaged fitting values, with all the compromises we know accompany that approach. Today’s top tier progressives are no longer limited by these assumptions. But no matter which progressive lens is fitted, ECPs should be aware of some latent aspects hidden in prescribing and fitting that can undermine wearer satisfaction with progressives.
PRESCRIPTION,
PLACEMENT AND POWER
Current free-form progressives offer quite a wide range of tailoring to ensure the lens being fitted best matches the wearer. From choosing a design’s hard or soft overall character, to the length and slope of the intermediate corridor, to the base curve desired, today’s advanced free-form progressives offer the most tailored visual performance ever available. Even so, eyecare professionals should always keep in mind some “external influencers,” those factors outside the design of the progressive that can impact wearer satisfaction as much as the chosen lens design.
PROGRESSIVES AND
THE PRESCRIBER
Perhaps nothing influences the degree of the doctor’s discretion in the final prescription more than time spent performing eyeglass rechecks. By the time a wearer lands in the doctor’s chair for a recheck, it usually means that the Rx has risen to be the top suspect behind their eyewear dissatisfaction. Although delivering the best progressive eyewear is a process that begins with an accurate refraction, it sometimes goes awry when well-intentioned prescriber discretion influences the final Rx
in ways that works against patient satisfaction. During progressive troubleshooting, ECPs should be aware of these areas that can unknowingly impact progressive satisfaction:
A. Massaging the astigmatism: Clearly, full correction of astigmatism delivers the best bang for the buck when chasing optimal acuity. But prescribing the full astigmatism can come with a price: a change in habitual perspective that can negatively impact comfort for more than a few wearers. For this reason, prescribers often reduce or eliminate minor amounts of astigmatism, up to 0.50D. Additionally, orthogonalizing the axis, the act of adjusting it to the prime meridians of 90 or 180, is also used to further reduce perspective side effects. But all progressive lenses possess some amount of residual astigmatism distributed across the lens surface. This astigmatism can negatively interact with any uncorrected refractive astigmatic error to decrease visual acuity and utility. Recommendation: Prescribe the full cylinder found and avoid orthogonalizing axis. Although satisfaction here is not guaranteed, the prospects for progressive success almost always improve when the eye’s astigmatism is properly and optimally corrected. If the wearer experiences perceptual discomfort tracked to their astigmatism correction, try switching to a softer design progressive.
B. Maximum plus and maximum acuity: Approach this timeless recommendation with caution. First, as the standard exam distance set at 20 feet, which equals a vergence of +0.16D, the difficult to discern final subjective lens choices could easily flip into an over-plus situation, clearly undesirable for driving and other far distance considerations. Further, anything that compromises on-axis acuity will almost always degrade peripheral acuity in progressive lenses. Recommendation: Trial frame the Rx outdoors to discover the optimal Rx for driving.
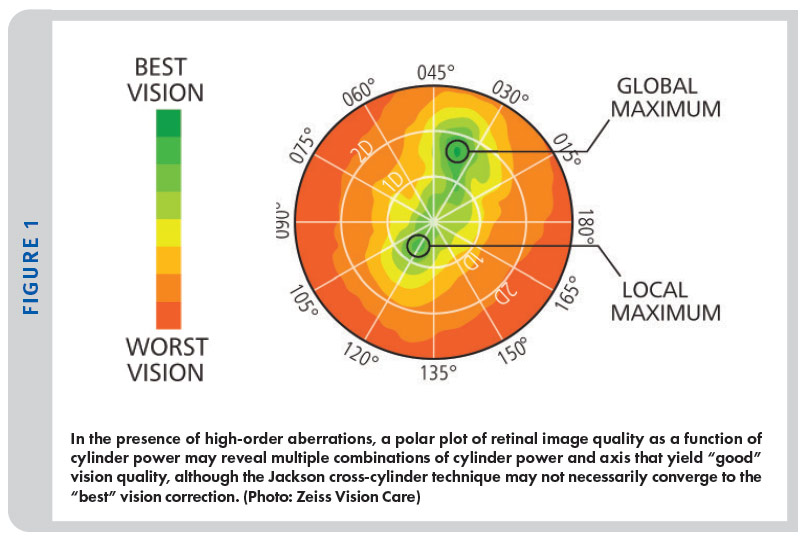
C. Be aware of pupil sampling: Pupil size controls more than luminous flux and near vision depth of field: The eye’s pupil size is the aperture stop that determines both the volume of light entering the eye and the effective cross-sectional area of the eye’s refractive elements—cornea, crystalline lens and retina—that are contributing to the final refractive result. Zeiss has recognized this effect and analyzes the focus across varying pupil sizes in their I.Profiler auto refractor instrument. Because of this, sphere power, cylinder power and axis can all vary between a daytime pupil of 2.5 mm diameter and a nighttime pupil of 5.5 mm or greater diameter. Recommendation: Again, trial frame the Rx outside the exam room, particularly at night if possible. The best correction for night use might be different enough to recommend two different prescriptions. (See Figure 1)
PROGRESSIVES AND THE FITTER
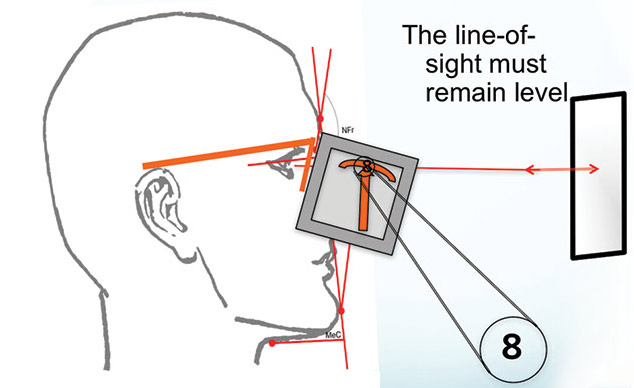
Progressive lens designers expect their lenses will be fit according to the recommended conventions, where the fitting cross of the lens is placed over the center of the pupil with the facial plane vertical—meaning perpendicular to the floor. This is also the proper head alignment for measuring the pantoscopic tilt of the frame chosen.
These are several interrelated factors to keep in mind when fitting a progressive:
A. Posture: A patient’s habitual headposture must be taken into account when specifying a fitting height. Habitual head posture reflects the routine manner in which an individual carries their head, i.e., facial plane tilted forward or back—with tilt-back posture posing more significance in progressive fitting. An alternative approach would be to adjust the fitting height to compensate for these postural deviations. Additionally, the corridor length can be adjusted as well, with longer corridors used for the head-back tilt and shorter ones employed in head-forward postures. An example of a combined approach might lower placement of the fitting cross by 1 mm to 1.5 mm and compensate the reading area position by specifying a 1 mm to 2 mm shorter corridor.
B. Corridor length: Today, issues arising from widespread mobile phone usage have required revising the traditional eye depression angles from 26 to 28 degrees, to a less severe 22 to 25 degrees. But as corridor value is often defined differently between lens manufacturers, comparing corridors between different designs will continue to remain a challenge. For example, manufacturers may use either a varying metric of 85 percent, 95 percent or 100 percent of add power to define the length of a lens’ corridor.
C. Frame fit: To further complicate achieving the best placement for a progressive, things such as patient preference for a loose frame fit, eyelash clearance, and sinus or skin sensitivity may require modifying the fitting height from its default position in front of the pupil. Indeed, wearer preferences maybe remain the most challenging of all variables in dispensing progressive lenses.
D. Pantoscopic Tilt: Targeting a proper pantoscopic tilt between 8 and 10 degrees, as measured in accordance in the above figure, is important when fitting a progressive for two reasons:
1. Proper pantoscopic tilt more properly aligns the image shell created by the lens with another shell, the uncorrected eye’s far point sphere. By tilting the lens, we optimally place the corrected eye-lens image on the retinal surface. This creates a “best balance” alignment for the lens’ focus across the primary field of view, both up/down and left/right. This alignment is precisely why we follow Martin’s Rule of Tilt: Lowering the optical center of a SV lens by 0.5 mm for every degree of pantoscopic tilt helps to position the lens’ optics for the largest area of clear vision.
2. Fitting ophthalmic lenses with a recommended tilt of 8 to 10 degrees, together with a frame whose wrap angle that does not exceed 4 to 5 degrees, helps minimize variations in lens-to-eye vertex distance across the eye’s full field of view and not just in the straight ahead/primary gaze direction. By reducing variations in vertex distance across the lens, variations in image magnification and prism are also reduced. This maintains optimum binocularity and reduces the swim experienced by sensitive wearers.
THE IMPORTANCE OF VERTEX
Historically, a vertex distance (VD) value is taken in situations where the fitted glasses are expected to depart from the normal 12.5 mm to 13.5 mm distance used in the exam room. The Rx threshold at which VD adjustments are used is between 5 and 6 diopters. The problem is that vertex distance is more than just a power dependent variable. Fitted vertex distance is used by lens companies to factor what lens areas need prioritization for correction, depending on the field of view (FOV), eye gaze or head angle. Lenses such as EssilorLuxottica’s Varilux X, Shamir’s Autograph Intelligence, IOT’s Endless Steady and Zeiss’ Individual Smart Life have further enhanced the gaze angle consideration by tracking and collecting data on how we use our eyes and interact with our devices on a daily basis.
A second important aspect of the fitted vertex distance of glasses is how this value, together with the refractive error of an eye, can be used to more accurately predict the eye’s Center of Rotation, or CoR. Hyperopic eyes typically have an axial length shorter than “normal” and vice versa for myopic eyes, but this is not always the case. When a moderate to stronger hyperopic Rx is fitted at a closer or farther than normal vertex distance, the resultant impact on effective power requires compensation. But the center of rotation of that eye and Rx will also not lie near its textbook position. Without more robust and exact measurements, the working assumptions we’ve used for the position of any eye’s CoR can be deeply flawed.
PROGRESSIVES AND
COMPENSATED POWER
The concept of compensated powers has been around since the dawn of free-form technology, yet continues to remain one of the most misunderstood aspects of today’s progressives. From my perspective, one reason compensated powers often perplex ECPs is best understood by looking at the common equipment and standards that are still taught and used to check lenses. Before the 1990s, high-precision lens meters, models capable of reading powers to a hundredth of a diopter, were simply not found in your average lab or optical shop. Going back to the first ANSI Z80.1 ophthalmic lens standard, issued in 1964, we see a stated power tolerance of 0.06D. This was based on the idea that the working production tolerance should be half the human eye’s just noticeable difference, the JND of 0.125D, also known as an eighth of a diopter. A manufacturing target of a 16th diopter precision was thought to be the limit of what could be accomplished with glass lenses and spherical grinding tools. But in reality, verifying lenses to this 1/16 diopter precision is not possible using a human operator and a
manual lens meter, because this combination of man and machine can never demonstrate repeatable readings at this level of precision. So, the idea that an ECP of that period could
measure or observe a lens’ power changing by hundredths of a diopter was essentially ridiculous. But not observing power changes arising from well-intentioned lens tilts doesn’t hide the
fact they’re still happening. If you couple this lack of awareness to a lack of wearer complaints, it’s no wonder ECPs can’t appreciate the power compensations presented on every lens verification slip.
WHY LENS
COMPENSATIONS MATTER
We all know patients who are very sensitive to a change of 0.25D sphere and a few more who demonstrate sensitivity to a 0.12D change. Further, within the timeframe of a career, some of us will encounter a handful of patients who are sensitive to even smaller differences in sphere, cylinder power or axis. Some of these micro-sensitivities have been connected to the state of the precorneal tear film, as it is the first surface to refract light incoming to the eye. The precorneal tear layer is said to have a dioptric influence of 0.12D, so it’s no wonder why people suffering from dry eye often complain about unclear vision. But whether or not there is an absence of complaint or sensitivity to small prescription differences, never forget that the eye is continually sensing where best focus lies, using a precision far finer than a noticeable difference of 0.12D. Perhaps this is why, more than we have acknowledged so far, those 0.01D free-form lens compensations can really matter, and why eyeglass wearers really do see and sense how the finest lenses deliver the finest vision.
UNDERSTANDING SPECIALIZED PROGRESSIVE LENS DESIGNS
Lenses such as Shamir Autograph InTouch, which introduced a non-linear, variable-slope progressive corridor to better manage screen use and mobile devices, and Zeiss’ DriveSafe, which rethought the starting point of the progressive corridor to help ensure superior night and driving vision, represent only the tip of the iceberg in what’s possible when tailoring an activity targeted design. Today, many more specialized designs have entered the marketplace. Let’s look at a couple of unique and specialized free-form progressives:
1. Anisometropia and the Shaw Lens: Shaw lenses are designed to optimize dynamic prism and dynamic magnification, which represent the differing prismatic and magnifying binocular effects an anisometropic wearer experiences as they gaze across their lenses. Binocular optimization of these prescriptions can be achieved using steeper or dissimilar base curves, differing lens thicknesses and the power of digital design and free-form manufacturing to improve fusion and reduce swim. But the finished cosmetics of these lenses can depart from accepted norms. However, wearers report the experience of wearing these lenses is fantastic, with many commenting they are enjoying real progressive comfort, perhaps for the very first time. Shaw progressives are an example of a true specialty approach and employs an advanced global iseikonic analysis in achieving high binocular optimization. The alignment of the chosen frame, i.e., its position of wear, becomes a very important part of the fitting parameters when binocularity becomes complicated, even in mildly anisometropic prescriptions.
2. Optimized eye teaming with Neurolenses: As many people have to work all day using various display technologies, ranging from phones to tablets to desktops, more and more find themselves suffering from headaches, dizziness, and head and neck strain often caused by small undiagnosed eye misalignments—the type which can be easily overlooked during most routine eye exams. Using the Neurolens Analyzer, these minor misalignments are both uncovered and precisely quantified. And fulfilled with Neurolens glasses, more optimal eye teaming, tracking and synching is restored using Neurolens’ ability to contour, or vary the amount of prism need in distance, intermediate and near tasks. The result for many sufferers is true visual comfort, perhaps for the very first time.
BECOME A PROGRESSIVE PRO
To best serve the contemporary eyewear
consumer, who today has far more channels to purchase products and explore information than ever before, an eyecare professional must always position themselves as the top choice for those who seek the most tailored and personalized product recommendations. To do this, it is imperative that local ECPs be seen as a trusted entity in their communities. But if your consumer-facing messages are mostly centered on sales, discounts or product specials, which are all a prospective buyer sees, I have a reality check for you: Online will always eat your lunch. Considering the overhead of maintaining a brick-and-mortar store, there’s just no logic in positioning yourself based solely on price. Luckily, one of the quickest paths to gaining trust is easy: Be open to help any eyeglass or sunglass owner with a problem, no matter where they’ve purchased their glasses. If you’re lucky, unhappy people will contact you, seeking help. By using your expert knowledge to successfully troubleshoot their problems, they will be both impressed and inclined to feel indebted to you, and helping them, without a chip on your shoulder about where their progressive glasses have been bought, is absolutely one of the best ways to earn their trust.
Even better, when that consumer is ready for their next purchase, they’ll be far more interested in your recommendations and far less interested in your prices. But to fully master today’s progressives, you must accept the fact that not every recommendation you make will be successful. But by remaining open and willing to tinker, periodic failures become the seminal opportunities to learn about and master what today’s advanced free-form lenses can really do. With a client’s trust in hand, you’ll become their “eye guy” for all things optical. Whether you are recommending a top tier general purpose progressive or are introducing a variety of specialized activity-focused lens options, the most important goal will remain to help your patients choose wisely. By focusing on the consumer, rather than some arbitrary sales goal, you’ll begin to enjoy both your job and your increasing healthy bottom line.
ESSENTIAL TECHNIQUES FOR DISPENSING
TODAY’S PROGRESSIVE LENSES
A PRIMER ON THE HISTORY OF PROGRESSIVE DESIGN
To fully appreciate what today’s free-form progressives can offer, and to understand what rules of thumb for fitting them no longer apply, let’s review this primer on the evolution of progressive design.
PROGRESSIVE DESIGN: 1950S TO 1980S
Early progressives, such as the original Varilux (now Essilor) of 1959, came with substantial undesirable astigmatism in the transition zones near the progressive umbilic. This was because the original Varilux was the uber of hard-design progressives. It is important to realize that the impetus for overcoming the production challenges of making a variable aspheric surface were driven by the want of the public to get rid of the telltale segment line as a sign of age, dependency and deficiency as it was to deliver a seamless visual experience to presbyopes of the day. As progressive lenses evolved during the 1970s and ’80s, the main goal of improving their design became reducing this astigmatism. This residual astigmatism was believed, at that time, to be the main culprit behind progressive dissatisfaction and non-adapts. The different approaches were best exemplified by the differences between the second generation Varilux and its main market rival, American Optical’s TruVision Omni. The approach of Varilux Infinity was based on a multi-add design that favored adjusting corridor length to optimize the increasing astigmatism gradient accompanying by increasing add powers, thereby optimizing corridor width and reducing related astigmatism swim-related effects. The other approach, exemplified by AO’s Omni, dispensed with retaining areas of stable power and surface curvature almost all together and spread out the surface astigmatism gradient throughout the entire lens through its unique bi-polar design. Nether design approach ultimately garnered sustained success for two reasons: Infinity required differing and sometimes uncomfortable eye rotation angles, especially in higher add powers, while those wearers uncomfortable with Omni found its bi-polar design delivered insufficient areas of clear stabilized prescription power. But one thing Omni wearers did find attractive was it reduced swim effects emanating from its inherently soft design. Omni became the choice of wearers sensitive to swim effects, those suffering from some degree of vertigo and pointed the way to how residual astigmatism and magnification effects might be better managed. Eventually, progressive design evolved from monocular optimization of optics to a fundamental consideration of binocular needs. Zeiss’ Horizontal Symmetry, which debuted in their Gradal HS, was amongst the first progressive lenses to address the importance of optimizing binocularity.
PROGRESSIVE DESIGN: 1990S TO 2000S
Front surface molded progressive designs had more or less plateaued in the early 1990s. But a dramatic change in frame styling, which harkened back to the much smaller symmetrical and classic designs of the 1930s, ushered in an urgent need to create progressives that would fit these new, narrower B shaped frames. Fitting heights as low as 11 mm and 12 mm were targeted, and these new “compact” designs featured significantly more surface astigmatism, especially in high add powers. The degraded peripheral distance vision was compensated for, in part, by the much smaller eye sizes. Despite their inherently poor optics, these compact designs achieved good acceptance by the wearers of the day. In the middle of all this, free-form lens technology, originally patented by Seiko in 1987, began to enter the marketplace in large part through the efforts of Zeiss and Schneider Technology, whose patents covered making free-form technology ready for production. But free-form progressives did not really begin to take hold and flourish in the market until the later 1990s and early 2000s.
With the benefits of a fully variable free-form surface in hand, first generation free-form progressives showed how surface astigmatism and binocularity could be further optimized. Still, there remained a tendency to favor the tradition of using longer corridors where possible. At the same time, the pressure for more cosmetically-favorable lens profiles drove the use of ever-flatter base curves. At this point, progressive design was ready to embark on a fundamental shift away from its legacy of an optics-only pedantic approach to a more outcome and wearer-centered approach.
PROGRESSIVE DESIGN: 2010S TO 2020S
Outcome-based visual satisfaction became the target goal of progressive lens designers. Except to advance beyond mere wearer satisfaction would require more sophistication in free-form lens design, manufacturer and real-world data patient about how people used their eyes on a daily basis. Further, the metrology of fitting eyewear—how eyewear is measured and fit— would need some major advancements. In consideration of this, the one-size-fits-all progressive approach is beginning to be laid to rest. Even wearer trials, the benchmark used to validate a preconceived design approach and long a staple method of a design’s validation, are being rethought. The expense and time needed to conduct a traditional trial is beginning to be supplanted by the use of artificial intelligence, or AI, to comb large user data sets and recognize not only the real-world usage patterns shared by all wearers, but also to create a hierarchy of important elements common in more activity-specific uses.
During the latter half of the last decade, the most advanced of today’s progressives have resulted not from some preconceived or pre-imagined insight, but often from new information gathered by tracking how progressive wearers comprehensively interact in all aspects of their daily routine. Top tier all-purpose progressives like EssilorLuxottica’s Varilux X, Zeiss Individual Smart Life, Shamir Autograph Intelligence, Hoya ID Mystyle 2, IOT Camber Steady, amongst others, are the result of using AI to bypass the length and expense of the brute force approach to validating designs through traditional wearer trials.
ADVANCED BIOMETRICS: THE SEARCH FOR THE BEST PERFORMING PROGRESSIVE
As we begin to use the power of artificial intelligence to mine patterns from large data sets to help customize the performance of ophthalmic lenses, a technique well beyond what the human mind can accomplish, we need to consider that using position of wear (POW) fitting values alone may be inadequate or incompletely described all the factors that described the eye-lens relationship in a pair of glasses. For example, we currently measure frame wrap angle off the face rather than on. Even today, the proper way to measure a frame’s pantoscopic tilt is both misunderstood and incorrectly performed on a daily basis, if it’s measured at all. And vertex distance is still associated with the need to adjust lens power, rather than an important part of a formula used to locate the eye’s center of rotation. The German lens company Rodenstock, whose products are not currently distributed in the U.S., has been rethinking how we measure and fit a pair of glasses, as it chases its vision to make the perfect pair of progressive lenses.
As companies chase ever finer degrees of precision and lens correction, which some in the industry have said is a fool’s errand, one lens company thinks otherwise. Using a concept called Advanced Biometrics, Rodenstock is intent on measuring and questioning every rule of thumb or fitting assumption that stands in the way of delivering the best progressive lens humanly possible. In pursuit of this goal, they have designed a new instrument called the DNEye Scanner. Using this DNEye Scanner, Rodenstock claims to be able to more precisely measure a suite of internal eye biometrics:
- Corneal Curvature, or CC, including asphericity and those areas cross-sectioned by the pupil.
- Anterior chamber depth, or ACD—This is used to precisely locate the eye’s pupil.
- Crystalline Lens, or CL—Its location and surface curvatures.
- The Axial Length of the eye, or AL—Also used to help place the eye’s CoR.
ADVANCED BIOMETRICS: ABSOLUTELY OPTICS FIRST
Using all of the above, the Rodenstock algorithm calculates the precise position of the CoR. This information, combined with a good subjective Rx and precise fitting biometrics, including normal position of wear values and machine-derived PDs and heights, is entered into the LDS at the lab. The resultant freeform lens design represents Rodenstock’s claim as the finest progressive lens ever made. The performance of this biometrically-optimized lens includes very precise manufacturing, with special attention made to ensure that the polishing operation and even the application of anti-glare coating does not in any way detract from the target lens performance. Clinical researchers at Hannaford EyeCare in New South Wales, Australia, have found that wearers of these biometrically-integrated glasses, referred to as B.I.G., demonstrate a degree of hyper-acuity—a subjective acuity/seen through the BIG that exceeds that measured during subjective testing. There is a theory that these biometrically-optimized lenses are interacting with both the eye’s foveal and parafoveal regions, with enthusiastic wearers reporting extremely sharp, wide fields of view.
While using averaged values for position of wear has produced many happy eyeglass wearers, many ECPs, especially those who consider themselves attracted to the newest technology, feel that patients expecting the best performing lenses deserve the most advanced measurements that can be made. In this space, certainly one of the technology leaders is Rodenstock.
–BS
Barry Santini is a New York state licensed and ABOM certified master optician.












