
By Sarah McGoldrick
Children are spending more time in front of computer screens, leading to a rise in cases of amblyopia, also known as lazy eye. According to the World Health Organization, approximately 19 million children under the age of 15 are visually impaired, with 12 million of those affected by uncorrected refractive errors and amblyopia.
Amblyopia is a unilateral or bilateral decrease in visual acuity. It is caused by deprivation of form sense of vision during the critical period of eye development, usually during childhood, resulting in abnormal binocular interaction.
In the past, the most common treatment for amblyopia was patching. Covering the good eye forces the patient to use the weak eye and hopefully establish neural connections with the brain. New technological advancements and treatment protocols including new lenses and technologies such as virtual reality and eye tracking mean children no longer need to wear a patch to enjoy better vision.
Optometrist Peter Shaw studies the causes and treatments of amblyopia. It was this need for better treatment technology that led him to develop the Shaw Lens and establish the Shaw Lens company. He says during the pandemic many parents have delayed or avoided having their infant’s eyes examined resulting in many cases of amblyopia having gone undetected.
“Amblyopia is a secondary disorder, meaning it is the result of active inhibition of vision due to strabismus and or refractive anisometropia. This is due to the fact that the brain cannot fuse the images as one. The child then learns to suppress or ignore one of the images,” he says, noting the only way to find out if an infant or child has amblyopia is through a comprehensive eye examination by an optometrist or ophthalmologist. Ideally, this should be performed on all children before the age of 3.
Though amblyopia develops early in life, experience shows most parents don’t notice it. “These disorders are present at birth or develop in infancy. Device use is not a risk factor for the development of amblyopia,” Dr. Shaw says, adding he believes it is important to identify the exact cause of a child’s visual problems in order to prescribe not only the right lens but the right complementary treatments.
In the past, little consideration was given to the design of the corrective lenses prescribed for anisometropia with amblyopia, except that in moderate to extreme cases, the dioptric power of the stronger lens was often reduced to aid adaptation.
Dr. Shaw explains that the fundamental issue is that unless there are near identical images presented to both eyes, the brain will continue to suppress the image from the weaker eye. In fact, the brain is good at this.
PROMOTING THE DEVELOPMENT OF EYE TEAMING AND BINOCULAR VISION
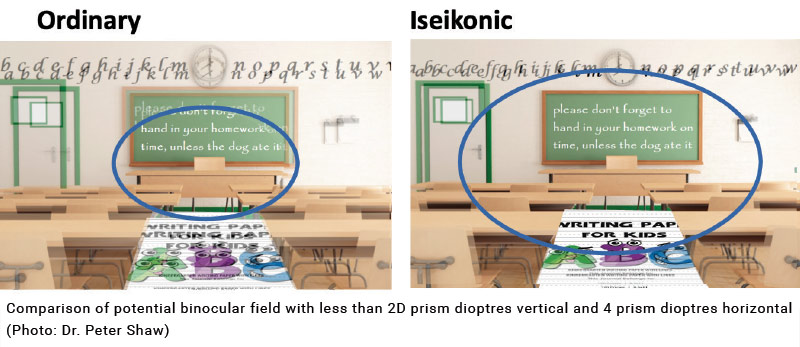
Iseikonic refractive therapy ensures that the ocular images are of equal size and clarity. This eliminates the trigger that causes the brain to suppress. Dr. Shaw states: “The only way to ensure a lasting cure for amblyopia is to promote the development of eye teaming and binocular vision; patching (a monocular therapy) does not aid in developing binocularity. Iseikonic refractive therapy provides a solid foundation for the remediation of amblyopia and in fact all binocular vision disorders.”
Shaw Lens, contact lenses, orthokeratology and refractive surgery are all examples of iseikonic refractive therapy suitable for the treatment of amblyopia. Shaw Lens therapy provides the necessary in the form of eyeglasses and is suitable for infants, children and those who prefer eyeglasses to the other forms of correction.
“Through the use of Shaw Lens, patients were able to experience significant improvement in vision,” Dr. Shaw says. “Monocular image blur was eliminated with the full refractive correction at distance and near, equal accommodation. Creating a solid foundation for eye teaming is fundamental in the treatment of amblyopia. This is what Shaw technology does,” he explains, adding the results are fast and permanent and patching is not recommended. “Shaw Lens treats the root cause of the most common type of amblyopia (refractive) by eliminating the image difference between the two eyes, creating an equally clear vision for each eye at distance and near, eliminating the image size difference or aniseikonia. The result is an elimination of the misalignment caused by the induced prism in off-centered gaze positions.”
Dr. Shaw notes that recent research points to the role of the visual cortex, indicating amblyopia is not an eye disease, but a disorder of the visual cortex, eliminating the binocular rivalry through the elimination of the obstacles allows the good eye to pull the bad eye along.
“This is proven through the analysis study of visually evoked potential through a process called binocular summation,” he says, adding studies indicate that binocular therapies, not patching, provide a better resolution of the condition and improved stereo acuity.
According to a 2015 study in the Journal of Clinical and Diagnostic Research, it was found that there is no critical period for the treatment in older (12 to 30 years) anisometropic amblyopia and that as little as two to four hours per day of occlusion of the better eye with thorough vision training near the visual task of amblyopic eye is effective. The study also indicated the importance of consistent compliance with patient therapy in order to ensure the best results.
Katie D. Fisher, OD, FCOVD is board certified in vision development and vision therapy. She says she has had many amblyopia cases presented to her where the previous eyecare provider suggested that there are no other forms of treatment beyond standard patching therapy at a young age. “It’s very frustrating that some doctors feel they can’t do something after a certain age,” she says.
Dr. Fisher believes this is the wrong approach to providing adequate care, and that eyecare providers should be seeking out the latest research literature and treatment options for all ages. She adds that some eyecare providers are relying on patching as the only solution without exploring the latest treatment approaches for amblyopia.
“We are learning that amblyopia is a binocular or two-eyed vision problem where the brain suppresses or ignores the image from an eye causing reduced clarity of eyesight in one or both eyes, and that the results of treatment from patching alone often do not last a long time,” she says, adding that blocking out all light and forms as well as peripheral vision with patching as the sole form of treatment can produce a negative outcome. “It can be detrimental. It can be difficult to get both eyes working together after that.”
Although amblyopia develops prior to about age 6 without treatment, and a monocular or one-eye approach to treatment with standard patching therapy is most effective for young children, the latest evidence-based literature has shown that a binocular or two-eyed approach to treatment is effective for all ages. A binocular approach to amblyopia treatment involves: 1. Prescribing contact lenses or Shaw Lens instead of regular glasses lenses to equalize the image size the brain receives from each eye when there is a difference in prescription between the eyes, and 2. A progressive program of doctor-supervised office-based vision therapy utilizing specialized computer and optical devices such as lenses, prisms and filters to improve the connection between the eyes and brain in order to treat the underlying suppression. One important vision therapy technique used in the binocular treatment of amblyopia is monocular fixation in a binocular field (MFBF), where one eye perceives detail and the other eye perceives background. During MFBF, a patient can use both eyes but receives feedback if the image from an eye is suppressed by the brain.
Dr. Fisher suggests that eyecare providers seek out information on the latest amblyopia treatment options available and co-manage with doctors that provide this form of treatment to ensure patients are getting the most effective care.
Dr. Fisher says children are using digital screens more than ever and that the recent pandemic brought the impact of screen time on vision performance when learning to light for many parents. She notes that most kids don’t use textbooks the way they did in the past, and that screens are now the main instruction method in many schools.
The effects of amblyopia can be alleviated with an annual comprehensive vision and eye health exams along with the latest forms of treatment. Dr. Fisher recommends a reduction in “leisurely screen time” and doing more paper-based work. She also recommends improving visual hygiene during prolonged near work by abiding by the 20-20-20 Rule, every 20 minutes take a 20 second break and look 20 feet away, and maintaining Harmon Distance, calculated by placing a closed fist under the chin and then holding a book at the tip of the elbow.

APPLYING VIRTUAL REALITY AND EYE-TRACKING SOLUTIONS
Charles Shidlofsky, OD, FCOVD has been utilizing vision therapies in the treatment of amblyopia at his Texas practice for years. Board-certified in vision development and vision rehabilitation, Dr. Shidlofsky has had the opportunity to explore many treatment options in order to provide effective and lasting treatment of amblyopia in children.
He believes the recent pandemic and increased use of computers has caused a significant increase in both physical and emotional stress on children. “There has been a rise in depression and anxiety, and the visual consequences can create a big effect. Parents are realizing their children are struggling,” he says, adding his practice had to create a waiting list to handle the backlog of patients who need to begin vision therapy. “The eyes are forced to accommodate and converge for so many hours a day, creating double vision.”
Dr. Shidlofsky is concerned by the rise in cases of myopia too over recent years. Cases in children were expected to double by 2050, however, he says the rates have already met or exceeded this long-range prediction. Cases remain at their highest in Asia but he notes there is an uptick of cases in North America and Europe where children are spending more time in front of screens. He urges parents and educators to make time for breaks away from screens and to book an appointment with their eyecare provider if they discover their child is having vision problems, adding that there are now excellent myopia management techniques available to us to slow the progression of myopia.
The treatment options for amblyopia continue to become more sophisticated and effective. One approach which is being pioneered by the Israeli company NovaSight uses eye tracking technology. The company’s CureSight binocular treatment, which is distributed globally by EssilorLuxottica, uses eye tracking to help children develop stereoscopic vision (see sidebar). Supported by an integrated cloud platform which processes data from the company’s CureSight system, the eyecare provider receives a comprehensive patient vision summary. Progress reports and real-time monitoring of the child’s treatment are easily accessible.
Other popular amblyopia treatments use virtual reality (VR) technology. Dr. Shidlofsky says two VR-based therapies, Optics Trainer and Vivid Vision, are excellent choices for ODs looking to provide their patients with better treatment.
The Optics Trainer VR system displays targets to the weaker eye while hiding them from the strong eye. This helps strengthen the weaker eye and promote eye teaming. Vivid Vision uses similar technology to help strengthen the eyes and improve focus.
Optics Trainer founder Josh Li has been helping kids see better through cutting-edge therapy, training and testing solutions utilizing eye-tracking and virtual reality technology. He says the recent pandemic has created an increased demand for his technology as more children spend time in front of screens; however, parents are taking advantage of the in-home component of the technology.

“The pandemic resulted in many patients not wanting to go into the clinics for safety reasons, as well as clinics reducing their office hours due to lower in-office visits,” Li says. “Many offices actually reported less usage of the technology due to increased sanitation requirements for the headsets. For the clinics still in operation, we saw an increase in at-home therapy.”
Li believes the in-home visual therapy support allows eyecare providers and parents to work together to improve results.
“This addresses sanitation concerns as well as reducing the frequency of in-office visits. With home therapy, doctors can monitor their patient activity and adjust their prescription remotely,” Li says, adding patching is no longer the go-to resource for eyecare providers. New technology has made treating amblyopia and other childhood eye conditions more effective. “Although patching has its benefits, patching does not promote eye-teaming (the ability for the eyes to work together). There are benefits to patching to strengthen the weaker eye, but there is also a need to train the eyes to work together again.”
Li and his team are continuing to develop more technology to assist with specific markets in vision management. He believes virtual reality will be an important part of vision care and rehabilitation as the industry continues to explore new therapies.
“We are working on specific tools for other markets such as sports vision, occupational therapy, physical therapy, pain management, and health and wellness. These are some of the many fields that we believe can benefit from Virtual Reality,” he says. “The biggest struggle ODs express to us is compliance. Therapy in the general public can be viewed as boring or tedious. Optics Trainer changes the perception of therapy. We offer tools that are not only fun, but effective and leave the patients wanting to come back.”
NOVASIGHT ASSIGNED THREE UNIQUE CPT CODES BY AMA FOR CURESIGHT AMBLYOPIA TREATMENT

NovaSight, a pediatric-focused eyecare company, recently took an important step toward establishing health insurance reimbursement for its CureSight digital treatment device for amblyopia when the American Medical Association (AMA) assigned three Current Procedural Terminology (CPT), or billing codes that are unique to the company’s technology. The assignment marked the first time the AMA awarded codes to an eye-tracking amblyopia treatment. The codes will allow physicians the opportunity to potentially be reimbursed for their services related to the use of CureSight in children with amblyopia and for patients’ health insurance plans to reimburse them for the treatment.
Additionally, NovaSight is sponsoring a randomized clinical trial that will generate data about CureSight for inclusion in an early 2022 510(k) clearance submission to the FDA, which could lead to the agency’s approval of the technology, according to NovaSight. Since June 2020, NovaSight has enrolled 67 of a targeted population of 90 children with amblyopia in the ongoing Israeli randomized controlled trial that for the first time as part of a 510(k) pivotal study is comparing vision outcomes with CureSight versus the current standard-of-care treatment using an eye patch. NovaSight is on track to initiate a supplementary trial this month for patients ages 4 to 9 in the United States.
NovaSight is pursuing the development of CureSight in addition to its commercially available EyeSwift vision assessment system, which is distributed globally by EssilorLuxottica
—SM
Sarah McGoldrick is a freelance writer who specializes in optical subjects. She is based in Toronto, Canada.












