
By Sarah McGoldrick
Since the start of the COVID-19 pandemic, there has been a major shift from the physical to the virtual world as we spend more time in front of screens for work, shopping and keeping in touch.
This has led to a rise in complaints of digital eye strain from patients caused by prolonged exposure to blue light. According to a July 2020 survey by global market research company Ipsos, a quarter of the respondents reported an increase in digital device usage during the pandemic, with the highest reported levels among those under 35 years of age. The poll found the number of people experiencing harmful effects from increased screen time is rising. Of the participants who report spending more time in front of a screen, 45 percent say they have experienced dry eyes, and 60 percent were concerned about the overall impact of screen time on their vision.
Children are also dealing with higher levels of digital eye strain and suffering long-term effects from increased exposure to digital devices. Research shows that low blue light levels may increase the chances of children developing myopia and nearsightedness.
Combatting the causes and effects of digital eye strain has left both researchers and vision experts divided over what is a safe level of blue light exposure. Since blue light is all around us and can offer many benefits to our health such as regulating circadian rhythm, it can be difficult to identify the source of discomfort. Exposure to blue light from the sun tells our body it is daytime, while the lack of light at night tells us it is time to get some sleep. Exposure to blue light during the night from digital devices tricks our body into thinking it is still daytime, subsequently disrupting sleep patterns and impacting overall health.
But what is considered unsafe? Natural sources such as the sun give off a rate of blue light exposure at 700 nm, while most digital devices give off well below this number ranging from 350 to 480 nm, leaving eyecare professionals and their patients questioning the science behind many blue light protection products.
Eyecare providers are demanding more research and proof of the effectiveness of recommended treatment options. There is also a call for improved education and a greater effort to better identify the causes of digital eye strain in order to provide better vision care.
David Salk, founder of Focal Point, a Berkeley, Calif., optical shop and CEO of eClips, a custom eyeglass clip maker, believes lack of education is one of the driving forces behind misdiagnosis and poor treatment of digital eye strain resulting from blue light exposure. He feels eyecare providers need to spend more time talking with patients to better identify lifestyle and work influences on blue light exposure. “Each person’s DNA and history of macular degeneration is different,” he says, adding everyone experiences a different reaction to their distance from screens, blue light exposure and hours spent on digital devices. “The best way to answer these questions is with more questions. If you are working in a retail environment with hundreds of LED lights or watching a lot of TV at night, you are going to get sleep disruption.”
Salk believes the industry has been focusing on the wrong narrative when it comes to both eyecare professional and patient education. He says companies need to be held accountable for the claims they make providing “quantification” of their protection claims. “We are providing them (ECPs) with narratives that are simplistic and designed to stimulate purchases. We should provide info and truth first,” he says, adding there needs to be standardization, which prevents companies from making potentially false claims.
Salk thinks lens manufacturers have over simplified the discussion of blue light issues rather than educating on the causes and prevention of digital eye strain symptoms. “Eyecare providers must become informed of the true science of blue light and not respond to marketing from lens companies who are providing coatings that do very little to address the problem.”
He points out there are no definitive studies that show computer screens and short wavelengths of blue light damage the macular. Instead, he suggests ECPs take a treatment approach that addresses patient comfort and prevention of the negative effects of blue light exposure, focusing on visual discomfort and accommodative stress.
Salk indicates there are many options for providing protection based on wavelength and environmental factors. He says shorter wavelengths create a host of issues including fluoz accommodation and contrast issues.
He believes that eyecare professionals should not automatically assume the information they are being provided with is accurate and should spend more time doing their own research, adding it is an uphill battle. “Eyecare professionals have to use critical thinking, and you have to be curious. They have to learn more and get better.”

ECPs should encourage patients to consult their optometrist or optician on the right lenses to help solve their digital eye strain
FINDING THE RIGHT PROTECTION
Many lens technology manufacturers offer UV protection solutions designed to let in the right amount of “helpful” blue light while filtering out the “harmful” radiation. But medical professionals are advised to do their research before advising patients to try blue light lenses.
A study published in An Bras Dermatol, an official publication of the Brazilian Society of Dermatology that analyzed the levels of radiation of lamps, TVs, tablets and computers, found monitors of commonly used electronic devices do not emit ultraviolet radiation that poses a risk to the population.
Studies like this are why Katharine Funari, OD, a faculty member at Johns Hopkins School of Optometry, stresses the importance of ECPs taking a science-based approach to choosing lens solutions for their patients. “There is no research in humans that shows exposure to blue light affects us on a long-term basis,” she says, adding ECPs should remind their patients about the 20-20-20 rule of taking a break, looking away from the screen and focusing on an object 20 feet away. “For their general well-being and posture, it’s important for patients to experience that break.” She adds if patients are feeling a lot of strain, they should be advised to reduce the intensity of light and use settings on their phone such as “night mode” on their digital devices.
Funari believes, because research is still in its infancy, it is difficult to determine what level of exposure to blue light is harmful. She notes studies have shown that kids who spend more time outside in natural sunlight experience less progression of myopia than those who spend more time inside. “It’s hard to say whether it’s blue light versus other factors that cause these issues. There is more natural blue light in the atmosphere, and research shows that outside time decreases the risk of becoming nearsighted,” she says, adding she takes a very cautious approach to treat digital eye strain. She goes on to say she “doesn’t prescribe blue light lenses’’ because it is hard to gauge how much light is being filtered through. Instead she offers them as potential solutions based on her patient’s symptoms.
Funari encourages eyecare professionals to question companies who offer any blue light technology to ensure patients are getting the right lens for their specific situation and not a one-patient-fits-all solution. “We are doctors, and it’s our job to educate and find unbiased research. We have to guide and educate patients so we can help them find the right product that works for them and provides our best medical care.”
Understanding a person’s lifestyle is one of the key factors of determining if over-exposure may be playing a role in eye discomfort. Robert Layman, OD, and acting president of the American Optometric Association, says he continues to look at new research on the effectiveness of blue light blocking lenses. He notes that overexposure to blue light may harm eye health, highlighting that UV rays from the sun can cause serious eye health issues including cornea damage, cataract development, pterygium, cancer and macular degeneration.
Layman says many factors determine how a patient responds to blue light exposure. He adds something as simple as eye color could have an impact on the eye’s response to blue light. “There needs to be more research. There is not enough clear-cut science to have a clear-cut policy. The science is still evolving.”
Layman recommends that doctors spend more time learning about their patient’s screen time habits with the influx of use during COVID-19, taking into account that all age groups are experiencing moderate to significant increases in digital device use. He adds that eyecare providers should not immediately assume digital eye strain as the cause of a patient’s eye issues and should still conduct a comprehensive eye exam to determine if the problem may lie with accommodation errors or convergence issues.
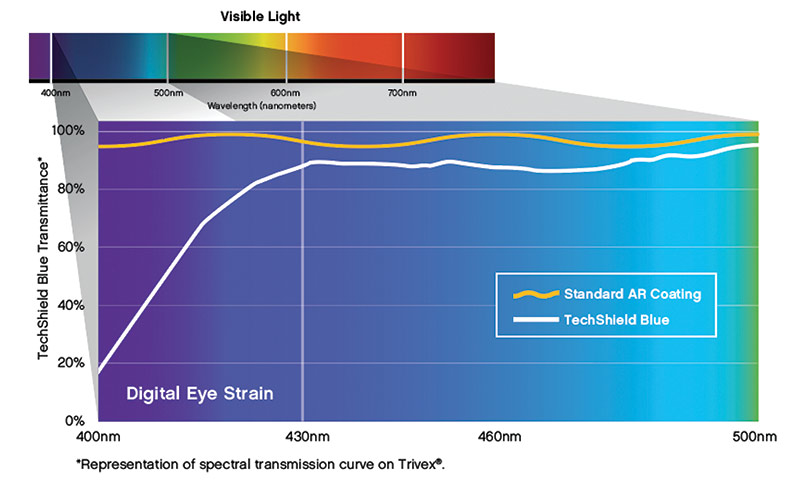
This spectral transmission curve for VSP Optics’ TechShield Blue with Trivex shows that it attenuates significantly more blue light between 400 to 430 nm, the part of the visible light spectrum that can cause digital eye strain, compared with standard AR coating
Layman suggests eyecare providers use the opportunity of discussing blue light technology to educate their patients on the importance of buying glasses from a reputable source. He says ECPs should encourage patients to consult their optometrist or optician on the right lenses to help solve their digital eye strain. “It’s not a one-size-fits-all recommendation. The difficulty we have is it’s a challenge figuring out the long-term effects for something that has only been around for the short term,” he says. “Part of digital eye strain can be related to visual functioning, and I would advise my colleagues to look past the hype of manufacturers making claims.”
Companies who develop blue light protection technology are spending more time in the research lab to ensure that the protection they offer is backed by science.
Mitsui Chemicals continues to develop lens technology that reaches further on the blue light spectrum. Ryan Rogers, marketing manager at Mitsui Chemicals says research needs to continue to look at how to prevent potential retina damage caused by digital devices. He notes the minimum standard for blue-blocking lenses should be in the range of a minimum of 400 to 420 nm, and that this protection will soon be enhanced with technology that can block light in the 450 to 460 range.
Rogers says Mitsui focuses on improving blue-blocking technology that not only deflects HEV light but absorbs the light for greater protection and decreases the likelihood of eye health issues. “We are always looking for health care benefits,” he emphasizes, adding Mitsui is always working on new formulations to improve both the level of protection and esthetic look of blue-blocking lenses. He notes many of the initial lens designs that came out as the eyecare profession began to address digital eye strain offered good protection, but the strong yellow dyes were a deterrent for consumers.
Jeffrey Harrell, senior director of product marketing for Essilor USA believes educating patients on the right options comes down to both the lens provider and eyecare professional. He says the Essilor team is proud of one of their most effective and best-known products Crizal Prevencia, which deflects up to 20 percent of harmful blue light from the sun and artificial light sources. He notes the increase in digital device use is not just impacting adults, but children as well. Harrell says eyecare professionals need to be aware of how both their older and younger patients are using digital devices in order to offer the best vision care.
Harrell feels the U.S. market continues to be under-penetrated when it comes to providing a wide selection of vision solutions for digital eye strain. He adds consumers are very conscious of lens aesthetics and will make choices based on poor residual color. This has forced lens manufacturers to develop technology that not only relieves discomfort, but also provides the visual look patients prefer. “The biggest challenge is how do you let the good light in without impacting aesthetics.” He notes Essilor has faced the same challenges as other lens designers. The residual color associated with blue light blocking lenses leaves consumers wary of exploring this lens technology. Harrell says patients are more aware of the technology but want a lens that looks good too.
“There is a growing consumer need and interest. We need to look at how we can partner with ECPs to increase awareness and offer them the right portfolio,” he says, noting it is important that ECPs get the proper training, messaging and tools to help their patients make an informed choice. “A patient is going to take to heart what an ECP recommends, they are not going to know a solution until it is offered.”
Alan Burt, vice president, product management and technical education at VSP Optics, believes the solution to digital eye strain is more complex than simple percentages and that a broad approach with a focus on understanding all facets of a patient’s lifestyle can help eyecare providers develop the right care plan. “We need to understand the patient’s lifestyle, visual behavior and environment to identify the nature and intensity of their blue light exposure: Is it a blue light-emitting device, or sunlight, or both?” he asks. “A blue-light-filtering lens product such as our TechShield Blue Anti-Reflective Coating may help improve visual comfort when viewing a lower intensity blue light source such as a digital screen because it targets blue light wavelengths associated with digital eye strain. A product such as our SunSync Elite Light-Reactive Lenses will provide this same benefit indoors and will also increase the amount of blue light filtration outdoors from sunlight to match the increased intensity of the source.”
Essilor’s Crizal Prevencia deflects up to 20 percent of harmful blue light from the sun and artificial light sources
He notes as medical device technology providers, a current scientific understanding of blue light exposure and how products align with the unique needs of individual patients is important. What patients would be the best candidates for this kind of eye protection? “To correctly assess if a patient would be a good candidate for a blue light-reducing lens product, eyecare professionals may use a questionnaire that allows the patient to identify their lifestyle needs. If a patient spends two hours or more in front of a digital screen indoors, a blue-light-filtering AR coating is worth discussing. If their lifestyle indicates they go between indoors and outdoors frequently, a light-reactive lens may be an option for continuous visual comfort throughout the day.”
He adds that the primary benefit of most blue-light-filtering lens products can be summarized as improving visual comfort. Burt also mentions there are minimum drawbacks to choosing blue light reducing lens products if the patient fits the symptom criteria but that all options should be investigated to find the right lens solution. “To ensure the best wearer experience, the patient’s lifestyle needs should be discussed to help determine the most relevant product and expectations set for the patient as to its performance.”
As this type of technology continues to develop, Burt is encouraged that patients will have even more effective solutions available to them. He adds that digital device manufacturers are also taking steps to help reduce digital eye strain in users, indicating a greater understanding of user side effects among the medical and tech industries.
“The current wave of blue light lens technologies that began around nine years ago has certainly reached new peaks in terms of commercial demand and available products; this growth has been accelerated by the recent changes to our visual environment for work, learning and recreation that are a direct result of the COVID-19 pandemic,” he says. “An interesting next wave that is starting to build is being propagated by digital device manufacturers, who are also identifying the issues and opportunities associated with blue light and starting to implement more device-based solutions; this doesn’t necessarily mean we’re seeing the end game for blue light-attenuating lenses. However, it does mean that we should endeavor to keep pace with the evolving science and technology of blue light to make sure we are providing patients with the most beneficial lens products for their evolving visual needs.”■
Sarah McGoldrick is a freelance writer who specializes in optical technology. She is based in Toronto, Canada.












