Photographs by Annie Gallagher
We all watch the “who done it” shows on TV and recognize the importance of fingerprints in solving the crime. Fingerprints are truly a useful tool in getting the bad guys, but in eyecare practices there are equivalent “clues” that are often overlooked or misunderstood. They are pressure marks. These little tattletales often lurk under the nosepads, behind the aricula (i.e. the portion of the external ear not contained within the head) or in the area of the mastoid process of the temporal bone. Fortunately you do not need to “dust” your patients or use those flashlights and orange glasses like those folks on “CSI” to detect these important clues.
Pressure marks related to spectacle wear fall into three categories: A. a discoloration of the skin related to heat build-up and possibly reduced circulation, B. a discoloration often accompanied by itching which results from an allergic response or hypersensitivity of the patient and C. a discoloration of the skin accompanied by a “weepy” appearance that may indicate a yeast involvement. Heat, excessive
pressure and other factors such as poor circulation (e.g. elderly patients or those with diabetes), microorganisms and sensitivity to frame or pad materials or residues of soaps, cosmetics, perfumes or other foreign material are all factors that can cause your patient to have annoying “pressure marks.”
A Dispensing ‘Tool’Pressure marks are uncomfortable to the patient, but they can also be a useful problem solving tool for the eyecare provider. A good example is the “never-ending dispensing.” We have all experienced these—usually early in our dispensing learning curve. Perhaps the dispenser feels that a textbook perfect alignment has been achieved and makes the mistake of asking, “Now, how does that feel?” The patient, having been asked to participate—and sometimes with no encouragement—offers suggestions like, “It’s a little loose on the sides of my head,” or “It doesn’t feel quite right on my nose.” This can lead the novice dispenser into prolonged and totally inappropriate changes in a fit that was already near perfect.
Rather than making patient-suggested changes, try recommending the frames should be allowed to “settle a bit” and then the patient should return after several hours (or a day or so) of constant wear so you can “read the pressure marks and refine the fit.” The patient should be cautioned that simply returning the next morning will not work because pressure marks tend to fade overnight. This “reading of the pressure marks” isespecially helpful because it presents objective evidence that will help you get the best alignment. It also gives good reason for your patient to keep his eyewear on long enough for adaptation to begin and it spares you from the frustrating experience of dealing with the complaints of patients who return carrying their new eyewear dangling from thumb and pointer finger like a dead mouse.
 What To Look For
What To Look For
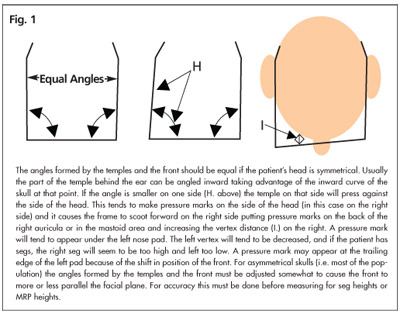
An example of classic pressure mark syndrome is a pressure mark under the left nose pad and another on the back of the right auricula or in the area or the left mastoid process (see Fig.1). Occasionally the pressure mark will show as a discoloration or even an indentation on the left side of the head in front of the auricula, in which case the patient will also probably complain of the eyewear “sliding down” because the skull often tends to taper narrower from the front of the ear forward and this taper shifts the frame forward and down the nose.
Analyzing ‘Pressure Marks’
We have all seen patients with sore spots that appear to be caused by the fit of their spectacle frames. They usually do need a frame realignment, but they return day after day. At first you relieve the pressure marks and soreness on the right side of the nose and in the left mastoid area. They return the following day with pressure marks on the left side of the nose and the right mastoid area and perhaps the soreness is either lessened or gone. The following day they return with no soreness, but with pressure spots on both sides
of their nose and in both the right and left mastoid areas. You make minor adjustments and, like the sun coming from behind a bank of clouds, they do not return for several days or longer.
Some time later this whole scenario repeats. You ask the patient where they have been and they tell you the last time you realigned their frame, you got it just right. They tell you they think they must have “bumped the frame” and now their problems have started all over again.
The next time this problem pops up, you might ask your patient if he has problems with shoes or dentures, and don’t be surprised if you get a yes. Patients with uncontrolled or undiagnosed diabetes tend to have problems with any pressure or rubbing on their skin when their sugar level is up. Although you cannot diagnose a problem with blood sugar level by the waxing and waning of mysterious pressure marks, you have a responsibility to suggest that the patient see his family physician about a possible blood sugar problem when you become aware of the above pattern of pressure marks and fit problems.
 Perhaps It’s Not Pressure At All
Perhaps It’s Not Pressure At All
Just as a jilted lover classically asking, “Has something come between us?” it is easy to overlook obvious oils, cosmetics, soap residues and other effluvia lurking between your patient and their eyewear. Sometimes it is a matter of teaching the patient to clean their frame daily with soap and water, and paying special attention to areas making contact with their skin.
Microbial action and allergic responses are encouraged by higher temperatures and the points of contact between the frame and the skin are actually insulated by the frame or pad material, preventing the release of heat. You may eliminate these problems by simple cleaning.
It is also important to recognize a few patients may be allergic to some frame materials. Changing the frame or “painting” it with a hypoallergenic coating to prevent skin contact may resolve this problem. Clear nail polish should not be used as a frame coating as it may prove to be an allergen to the facial tissue. Commercially available coatings such as BPI’s FrameGard should be used if you must coat a frame to reduce allergic reactions.
Acne Rosacea
In a study of more than 1,000 rosacea patients, over 80 percent indicated sun exposure as a trigger for rosacea flare-ups and about half of all rosacea sufferers experience ocular complications such as burning, dryness and grittiness of the eyes. This may argue for the importance of large, UV blocking, clear lenses and UV blocking sun lenses for these patients. However, rosacea can be exacerbated by a tightlyfitting bridge that increases vascular congestion. The result can be an increase in the severity of the rosacea in the nasal and central facial areas. This may be especially important if your patient has rhinophema (i.e., W.C. Field’s nose), a common rosacea complication. Provide rosacea patients with the lightest eyewear possible and then fit with minimal bearing on the nose.
Pad Marks of Long Standing
 Elderly patients in particular tend to have indentations and pressure marks resulting from many years of pad pressure on the same areas and these indentations and marks may persist even though the pad is perfectly aligned. If the shape of the pad is asymmetrical and if the attachment of the pad to the pad arm is about 30 to 40 percent from the top of the pad, you may be able to invert the pad to achieve
Elderly patients in particular tend to have indentations and pressure marks resulting from many years of pad pressure on the same areas and these indentations and marks may persist even though the pad is perfectly aligned. If the shape of the pad is asymmetrical and if the attachment of the pad to the pad arm is about 30 to 40 percent from the top of the pad, you may be able to invert the pad to achieve
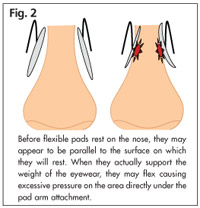
an alternative bearing area. It may also bepossible to move the pad by adjusting the pad arm. Larger pads might also be used for a “snowshoe” effect that spreads the weight over a larger area, but use these with caution because they may further insulate the tissue and the increased heat may promote more irritation. Another alternative that should be used with caution are soft, flexible pads. If they are too flexible, they may actually concentrate the weight-bearing part of the pad over a smaller area (Fig. 2).
An important rule for adjusting pads is to place bends on the pad arm as close to its attachment to the front as possible if you want to change the position of the front relative to the face. To change the position of the pad relative to the nose (e.g. higher, lower or more anterior or posterior) the bends need to be closer to the mid-section of the pad arm. Placing a bend close to the attachment of the pad arm to the pad will change the orientation of the pad on the nose. It is usually best to make the first bends close to the front and then work toward the attachment to the pad.
Frames with fixed pads such as the classic keyhole and saddle bridges can also leave inappropriate pressure marks, especially for patients who are at risk for these kinds of problems. In general it is best to lift the frame slightly and evaluate how well the bearing area of the fixed-pad frame parallels the surface of the nose. Unless the alignment is parallel, or nearly so, you may either have to reshape the bridge fit by attaching wedge pads, reshape the alignment by grinding or filing, attach adjustable pads or select a different frame.
The elderly, patients with histories of allergies, diabetics and those who allow their eyewear to become “unhygienic” are particularly at risk for serious complications triggered by the design and alignment of their eyewear. Coupling all this with hot weather and larger, heavier lenses and frames can lead our patients to unhealthy situations with discomfort, poor eyewear performance, skin lesions and general eyewear dissatisfaction. Fortunately, pressure marks can be among your most important clues when analyzing and correcting these issues. They provide meaningful information to optical sleuths and should never be overlooked.
Palmer R. Cook, OD, is director of professional education for Diversified Ophthalmics in Cincinnati.
Special thanks to Joan Wiss, MD, a Myrtle Beach, S.C. dermatologist, for her assistance in the preparation of this article.













