US
Pharm. 2006;6:34-38.
Each year in the United States, exposure to
excessive natural heat results in approximately 400 deaths, all of which are
considered preventable.1 In addition, about 200 Americans--most of
them 50 or older--die each year due to health problems caused by high heat and
humidity.2 The Centers for Disease Control and Prevention (CDC)
reported 3,829 deaths due to weather conditions between 1979 and 1999. Of the
3,764 deaths with a reported age, 142 occurred among children 4 years or
younger and 1,068 occurred among persons 75 years or older.3 During
that time frame, about 182 deaths per year were associated with exposure to
excessive heat due to weather conditions (annual deaths associated with
exposure to excessive heat ranged from 54 to 651 during these years).3
The body's inability to cope with heat,
i.e., the inadequate or inappropriate responses of heat-regulating mechanisms,
is often cited as the cause of such heat-related illnesses as heat exhaustion,
heatstroke, and dehydration. However, since deaths attributed to hypertension,
diabetes, and lung disease increase by 50% during heat waves, the risk of
heat-related death may depend more on the severity of the underlying disease
than on the severity of stress secondary to heat.4
Hyperthermia
An elderly person's body
temperature may rise when he or she is unable to rid the body of excess heat
or when the body produces too much heat, known as hyperthermia. When
air temperature rises above 98.6°F, the body gains excess heat and has
difficulty releasing it when concomitant high humidity makes evaporation of
sweat less effective.5 Seniors have more difficulty acclimating to
higher temperatures and humidity than do younger individuals. Even
temperatures in the low 90s can be very dangerous for older adults.2
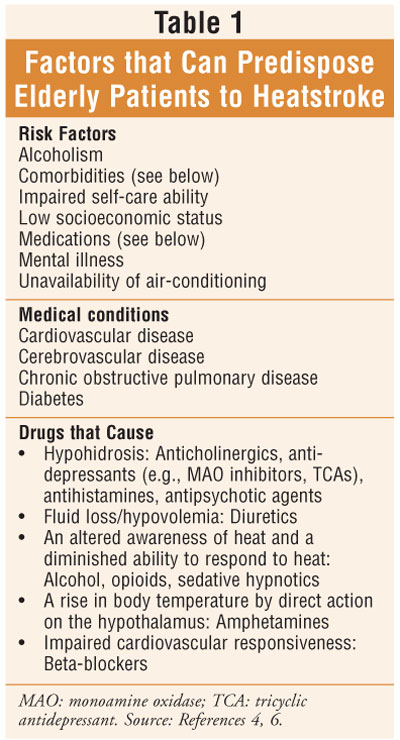
Additionally, certain medical conditions and medications may predispose
individuals to hyperthermia, complicating matters (table 1). Precautions
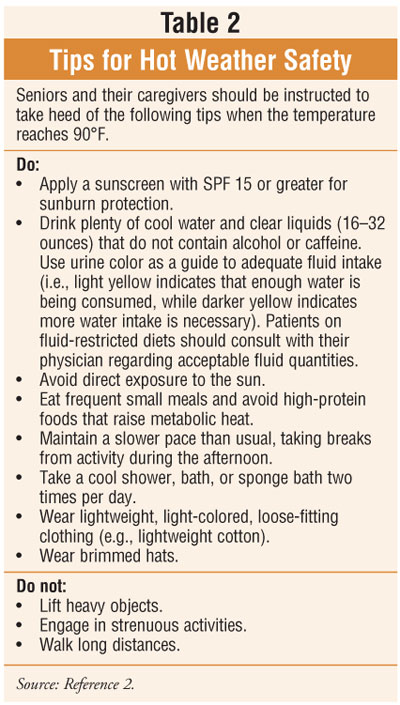
against hyperthermia include such commonsense recommendations as using
air-conditioning (e.g., in the home or at public venues), replacing fluids and
salts lost through sweating (drinking must continue even after thirst is
quenched), wearing light, loose-fitting clothing, avoiding strenuous exertion,
and misting or wetting the skin with cool water (table 2).5
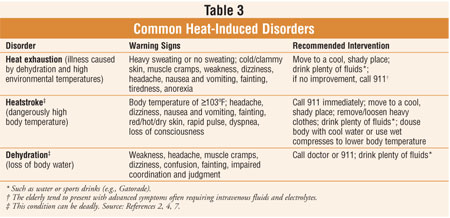
Heat Exhaustion
Heat exhaustion
is an illness caused by high environmental temperatures and dehydration (
table 3).2 The two major categories of heat exhaustion are water
depletion (producing hypertonic dehydration) and salt depletion
(loss of fluid and sodium chloride through sweating and replaced with
electrolyte-free water); the latter occurs in heat cramps.4
Treatment for seniors usually consists of intravenous replacement of fluids
and electrolytes based on abnormal laboratory values, since the elderly tend
to present late with advanced symptoms.4
Heatstroke
Heatstroke
is more common during summers with prolonged heat waves.6 During
hot, humid weather, heat exhaustion can progress to heatstroke if not treated.
Heatstroke occurs insidiously in the elderly, in whom the ability to dissipate
heat declines.4 In fact, people ages 65 or older are 12 to 13 times
more likely to experience heatstroke than are younger individuals.4
Heatstroke always involves a dangerously high body temperature (generally,
higher than 106°F or 41°C).5 While prodromal signs such
as dizziness, headache, and weakness may occur, loss of consciousness is
usually the first manifestation.4 Other symptoms and signs include
cardiovascular response (e.g., ECG changes); central nervous system
involvement (e.g., lethargy, stupor, coma); renal manifestations (e.g., renal
failure secondary to rhabdomyolysis); severe hypokalemia (thought to be
secondary to increased aldosterone secretion); elevated liver transaminases
(jaundice is common while hepatic damage is rare); and coagulation defects
(e.g., elevated prothrombin and partial thromboplastin; decreased fibrinogen
level).4
While many use the term heatstroke loosely,
the condition constitutes a medical emergency and requires hospitalization and
continuous monitoring.4 Risk factors, including use of certain
drugs and some medical conditions, may predispose a patient to heatstroke. It
is prudent, therefore, to obtain a thorough medical and medication history to
help prevent heatstroke or elucidate its cause.4 Increased public
awareness and prompt intervention by family members, caregivers, onlookers,
and health care professionals can reduce morbidity and mortality from
heatstroke.4
Dehydration
Dehydration is the most common
fluid and electrolyte disturbance in the elderly; hot weather is a common
contributing factor.4 A popular misconception is that a dehydrated
person experiences intense thirst. Thirst is an unreliable indicator of
dehydration because rapid fluid loss overwhelms the body's normal thirst
mechanism.7 Common symptoms include diminished coordination,
fatigue, orthostatic hypotension, and impaired judgment.
Diarrhea is a major cause of morbidity and
mortality in seniors because of a decreased capability to replenish fluid
losses and to tolerate intravascular hypovolemia associated with dehydration.
4 Seniors may be more susceptible to infectious diarrhea due to a higher
incidence of decreased mucosal immune function, luminal stasis (e.g., from
motility disorders or previous surgeries), or hypochlorhydria and achlorhydria
(e.g., from gastric acid–suppressing medications or pernicious anemia) in the
elderly.4
According to the CDC, traveler's diarrhea
(TD) is characterized by the fairly abrupt onset of loose, watery, or
semiformed stools associated with abdominal cramps and rectal urgency.8
Symptoms may be preceded by a prodrome of gaseous and abdominal cramping, and
additional symptoms such as nausea, bloating, and fever may be associated.
8 Vomiting may occur in up to 15% of those affected.8
Symptoms are generally self-limiting and occur abruptly during or soon after
an individual returns from travel. Attack rates are commonly reported to be
between 20% and 50%.8
The primary causes of TD are infectious
agents, which include enteric bacterial pathogens, viral enteric pathogens,
and parasitic enteric pathogens. Twenty percent to 50% of TD cases are
attributed to unidentified causes. TD risk is associated with the
categorization of the travel destination: high-risk, intermediate-risk, and
low-risk (see CDC Web site below).8
Prevention methods include strict attention
to food and beverage ingestion (e.g., drink bottled beverages and avoid
consuming products sold by street food vendors) and the use of
nonantimicrobial medications and prophylactic antimicrobial agents. The CDC
reports that adherence to restrictive food and beverage measures is difficult
for travelers, that antiperistaltic agents (e.g., diphenoxylate, loperamide)
are not effective in preventing TD, and that prophylactic antibiotics have no
effect on viral and parasitic diseases and may render a false confidence about
consuming risky food and beverages.8 Therefore, the CDC does not
recommend prophylactic antimicrobial agents for travelers, but rather,
sensible dietary practices as a prophylactic measure, since available early
treatment renders excellent results. In special circumstances, prophylactic
antimicrobial therapy along with a risk-benefit analysis is advocated for
travel.8 For the most recent recommendations for the treatment of
TD, see the CDC Web site at: www.cdc.gov/travel/diseases.htm#diarrhea.
Protection from Sun Exposure
Protection from excessive sun
exposure that might contribute to sunburn, medication-related photosensitivity
reactions, skin cancer, and heat-related illness is an important issue to
address with seniors. Sunscreens with a high sun protection factor (SPF) of 15
or greater should be applied to all exposed areas of the skin when outdoors,
and the use of long-sleeved shirts, long pants, and wide-brimmed hats is also
recommended.5
Information List for Safety
Another safety tip is for seniors
to always have a patient information list with them, especially when traveling.
9 The list should include, but not be limited to, name, address, and
allergies of the individual; emergency contact information; list of
medications (generic names included) and conditions for which they are being
utilized; and name, address, and telephone and fax numbers of primary
physician and pharmacy. It is also wise for seniors to consider wearing a
medical identification bracelet, if applicable.
Conclusion
Heat-related illness is a major
cause of preventable morbidity. During the summer, sustained exposure to high
temperatures puts the elderly at particular risk of suffering from conditions,
such as heat exhaustion or heatstroke, stemming from dehydration. Increased
public awareness of heatstroke and prompt intervention by family members,
caregivers, and health care professionals can reduce morbidity and mortality
of heat-related illnesses. Health care practitioners should advocate
familiarization with risk factors and preventive measures to patients, their
families, and caregivers.
REFERENCES
1. Semenza JC, Rubin CH, Falter
KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N
Engl J Med. 1996;335:84-90.
2. The American Geriatrics Society
Foundation for Health in Aging. The American Geriatrics Society's Hot Weather
Safety Tips for Older Adults. Available at:
www.healthinaging.org/public_education/hot_weather_tips.php. Accessed April 5,
2006.
3. Centers for Disease Control and
Prevention. Morbidity and Mortality Weekly Report. Heat-Related Deaths--Four
States, July-August 2001, and United States, 1979-1999. Available at:
www.cdc.gov/mmwr/preview/mmwrhtml/mm5126a2.htm. Accessed May 1, 2006.
4. Beers MH, Berkow R, eds. The
Merck Manual of Geriatrics. 3rd ed. Whitehouse Station, NJ: Merck & Co;
2000:562-563, 659-663, 923-930, 1085-1092.
5. Beers MH, Jones TV, Berkwits M, et
al., eds. The Merck Manual of Health & Aging. Whitehouse Station,
NJ: Merck Research Laboratories; 2004:
31-32, 385, 889.
6. Helman RS, Habal R. Heatstroke.
eMedicine from WebMD. Available at: www.emedicine.com/MED/topic956.htm.
Accessed May 1, 2006.
7. Dehydration and heat-related
illness. US Pharmacist. 2000;25:82.
8. Centers for Disease Control and
Prevention. Traveler's Diarrhea. Available at:
www2.ncid.cdc.gov/travel/yb/utils/ybGet.asp?section=dis&obj=travelers_diarrhea.htm&cssNav=browseoyb.
Accessed May 10, 2006.
9. Zagaria ME. Tips for traveling
seniors. US Pharmacist. 2005;30:32-36.
To comment on this article,
contact
[email protected].











