US Pharm. 2006;12:23-29.
The backbone of long-term care for senior adults in the United States continues to be the care delivered by family members. An estimated 79% of people who need long-term care continue to reside at home. 1 About 75% of family caregivers are women, and approximately 25% are spouses.2 Couples in which one partner cares for the other tend to be of disproportionately lower socioeconomic status.3 Approximately 26 million adults in the U.S. provide unpaid assistance to adult family members who have a disability or chronic illness.1 When we include caregiving delivered by friends and neighbors, the total number of unpaid caregivers increases to 44 million.4 According to one estimate, replacing the work of family caregivers with that of paid home health care staff would incur a cost to the nation of $45 billion to $94 billion per year. 5 In addition, caregiver services provided to loved ones, including home care, transportation, and financial management, would incur a cost of $257 billion annually.4 While the average age of a family caregiver is 43 years, 33% of caregivers are 65 or older.2 Seniors in our society are not only receiving care but delivering caregiving services as well.
In older patients, achieving therapeutic objectives (e.g., optimal health-related quality of life, outcomes consistent with a patient's personal beliefs and objectives) through the utilization of a particular approach to care (e.g., relief of suffering, cure when possible) may require the assistance of a caregiver. When a patient is faced with a specific illness, or when caregiving becomes necessary, important insight can be provided if the health care professional is sensitive to the social relations and family history of each individual.6 Furthermore, the need for long-term care placement for reasons such as caregiver burnout, dementia, problems performing activities of daily living, and urinary incontinence may be delayed if these problems are solved or avoided through a comprehensive understanding of caregiving. By intervening with compassion and providing information, resources, and support, pharmacists may positively impact senior care recipients and their caregivers.
Caregiver Burden
Family caregivers often juggle
various roles at home and at work and may experience health problems and
stress.7 Assisting care recipients with activities of daily
living (e.g., bathing, dressing, eating, toileting) and instrumental
activities of daily living (e.g., grocery shopping, meal preparation, money
management) can be physically challenging, emotionally overwhelming,
time-consuming, and expensive.
Emotions commonly felt by caregivers include anger, depression, fear, frustation, guilt, hostility, and shame.2 Caregivers may feel neglected, abandoned, isolated, and resentful. As a result, caregivers may become fatigued or act out inappropriately. Insomnia may also ensue. Although caregivers of older persons with a chronic condition or disability commonly experience stress and burden, health care practitioners should routinely assess family caregivers for stress-related health risks. 7 Stress associated with performing family caregiving tasks can result in an increased risk of infectious disease, depressive symptoms, and chronic illness such as diabetes, heart disease, and cancer.5 For example, family caregivers of cancer patients have shown higher levels of stress, burden, and diminished quality of life.8
In addition, family caregivers are less likely than their peers to engage in behaviors that promote health and well-being and therefore should be encouraged to engage in activities that prevent illness and support and benefit their health.5 It has been recommended that caregivers be examined before they experience any adverse effects. Collaborations on caregiving between health care providers and the aging network, in which family caregivers would be identified in the office of a primary care physician, should be considered.9
There is an elevated risk for clinical depression seen in caregivers of persons with cognitive impairment.10 Adult children experience more caregiver burden than do more distant relatives, when both groups care for community-dwelling, memory-impaired seniors, and adult daughters have greater caregiver burden compared to more distant relatives.11 One study examined health-related quality of life and overall quality of life of family caregivers of stroke survivors to determine changes over time and to identify quality-of-life predictors.12 Researchers found the most important predictors of quality of life were the stroke survivor's behavioral disturbances and reintegration into normal patterns of living.12 Those caregivers reporting fewer stroke-survivor behavioral disturbances and well-adjusted reintegration were the ones who reported a higher personal quality of life.12
Studies have revealed that many terminally ill patients never receive hospice care and late hospice enrollment can have deleterious effects on patients and their family members.13In the U.S., the median length of stay at hospice declined 27%, from 26 to 19 days between 1992 and 1998, and in a prior study of patients diagnosed with terminal cancer and using hospice, only one third enrolled with hospice within one week prior to death.13Recently, a study focused on caregiver perceptions of factors that might contribute to delays in hospice enrollment. The analysis of results identified three themes common to the experience of transitioning to hospice:
1. Caregivers' acceptance of the impending death,
2. Challenges in negotiating the
health care system across the continuum of care, and
3. Changing patient-family dynamics.
13
The researchers concluded that identifying these themes from the caregivers' perspective helps to formulate a hypothesis about why there may be delays in enrolling a terminally ill patient in a hospice program. This may ultimately be useful in designing interventions that are consistent with caregivers' needs.13
Long-Distance Caregivers
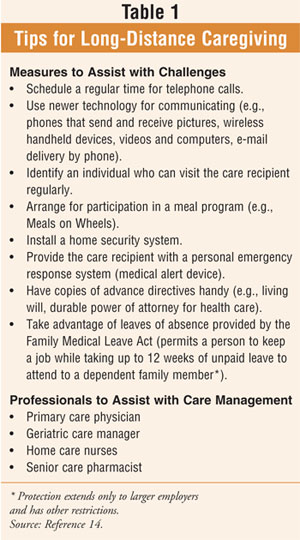
Long-distance caregivers, such as
adult children, face unique challenges that may include difficulty
communicating with a loved one or an incomplete or inaccurate impression of a
loved one's ability to perform daily activities.14
Family members may live hundreds to thousands of miles apart, which can
complicate efforts to coordinate and provide necessary, appropriate, and
timely care for seniors. Long-distance caregiving may provoke a feeling of
helplessness; however, there are measures that can be employed to assist with
the associated challenges, and professionals are available to assist with care
management (table 1). Angela Heath provides a list of strategies for
coping with long-distance caregiving in her book Long-Distance Caregiving:
A Survival Guide for Far Away Caregivers:15
• Get organized.
• Identify your informal network.
• Investigate travel alternatives.
• Discuss legal and financial issues.
• Take care of necessary paperwork.
• Tap into the aging network.
• Develop a plan of care.
• Adjust your plan of care when
necessary.
• Explore relocation issues.
• Take care of yourself.
Senior Caregivers
While older adults struggle with
the management of comorbidities, disabilities, and complicated medication
regimens, they often have the added responsibility of being caregivers
themselves. This can increase their daily challenges and contributes to their
decisions about their own long-term care.16,17 Many seniors develop
a preference for home care and avoid life- sustaining measures in formulating
their own advance care directives.18 Findings have shown that
caregiving accompanied by emotional strain is an independent risk factor for
mortality among seniors caring for loved ones.5 The role of seniors
as caregivers is underscored by the fact that in the U.S., approximately
640,000 individuals with mental retardation reside at home with senior parents
who are in their sixth, seventh, or eighth decade of life.1,19
Support for the Caregiver
Interventions aimed at improving
the coping skills of caregivers have been effective in improving caregiver
quality of life, by reducing the burden related to patients' symptoms and
caregiving tasks, compared with hospice care alone or hospice plus emotional
support.8 Structured caregiver skill-training interventions have
shown promise for caregivers even in the environment of end-of-life care and
for families already receiving hospice care.8 In some states,
caregiver support services are incorporated into programs that serve older
people or adults with disabilities, while in other states, caregiver support
is a separate program with distinct eligibility criteria.20
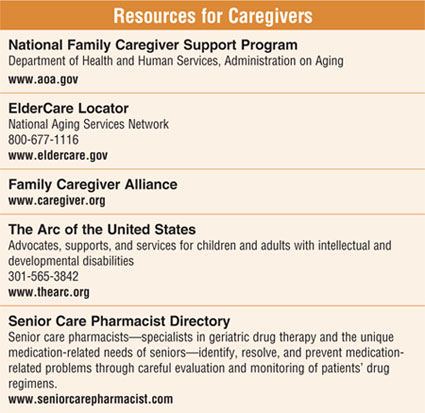
Once a family has decided to provide care in the home, the National Family Caregiver Support Program (NFCSP) may provide invaluable guidance and access to services. Supportive (e.g., counseling and family mental health services) and supplemental (e.g., home health care, adult day care, meal programs) services, provided either on a regular basis or as respite care for a block of hours or days, may allow a family to continue with caregiving responsibilities beyond what they would have been able to accomplish unassisted.16 Furthermore, the NFCSP has reached out to special populations and has responded to the unique needs of older persons and their families and caregivers. Those eligible for support provided by NFCSP are family caregivers of older adults (60 or older) and grandparents and relative caregivers of children 18 and younger. This includes grandparents who are sole caregivers of grandchildren and those individuals who are affected by mental retardation or who have developmental disabilities. Priority consideration is given to persons with the greatest social and econo -mic need and to older individuals providing care and support to persons with mental retardation and related developmental disabilities.
A Caregiver Tip Sheet, available through the NFCSP, provides advice and guidance on managing a caregiver's health. 4 The tip sheet includes recommendations on immunization (e.g., influenza, pneumococcal, tetanus booster), yearly check-ups, and cancer screenings (e.g., mammography) and encourages eating healthy foods, taking time to relax, exercise, and socialize, and reaching out for help and assistance from family, friends, neighbors, and local caregiver resources.
Summary
Family caregivers provide the
majority of the assistance that enables seniors to live independently in their
own homes and communities. The unpaid and informal care that is provided by
family caregivers is an essential source of help for elderly persons,
especially those who are disabled. However, caring for an older person with a
chronic condition or disability can be stressful and burdensome for many
family caregivers and often contributes to psychiatric and physical morbidity.
Additionally, more than one third of family caregivers are 65 or older, which
further complicates the challenges and obstacles observed among their younger
counterparts due to the complex of diseases and impairments faced by many
older adults. Health care professionals, including pharmacists, can
appropriately and effectively guide and advise caregivers on available support
systems and resources to assist them in this comprehensive role.
References
1. Singer P. Long-term care
system leans heavily on aging caregivers at home. Coshocton Tribune.
May 31, 2003.
2. Cora VL. Helping Family caregivers
of older adults with dementia. ElderCare. 2006;6(1):1-4.
3. Beers MH, Berkow R. The Merck
Manual of Geriatrics. 3rd ed. Whitehouse Station, NJ: Merck & Co.;
2000:92-93, 112-115, 142-143, 365, 376-377, 1412.
4. Caregiver Tip Sheet. Available at:
www.aoa.gov/prof/aoaprog/caregiver/overview/CaregiverTipSheet.pdf. Accessed
October 30, 2006.
5. National Family Caregiver Support
Program, Department of Health and Human Services, Administration on Aging.
Available at:
www.aoa.gov/prof/aoaprog/caregiver/careprof/TownHall/townhall_12_16_03.asp.
Accessed October 30, 2006.
6. Antonucci TC, Schulz R. Families,
social support, and caregiving. In: Hazzard WR, Blass JP, Halter JB, et al.
Principles of Geriatric Medicine and Gerontology. 5th ed. New York:
McGraw-Hill, Inc.; 2003:255-263.
7. Who's Caring for the Caregivers?
AARP Unveils New Report on Trends in Support for Family Caregivers.
Consumer-Directed Services for Caregivers Take Hold in States. Available at:
www.aarp.org/research/press-center/presscurrentnews/caring_for_caregivers.html.
Accessed November 20, 2006.
8. McMillan SC, Small BJ, Weitzner M,
et al. Impact of coping skills intervention with family caregivers of hospice
patients with cancer: a randomized clinical trial. Cancer.
2006;106:214-222.
9. Feinberg LF, Wolkwitz K, Goldstein
C. Emerging Trends and Practices in Family Caregiver Support. Research Report.
National Center on Caregiving, Family Caregiver Alliance. March 2006.
Available at: www.aarp.org/caregiver. Accessed November 20, 2006.
10. O'Rourke N, Cappeliez P, Guindon
S. Depressive symptoms and physical health of caregivers of persons with
cognitive impairment: analysis of reciprocal effects over time. J Aging
Health. 2003;15:688-712.
11. Chumbler NR, Grimm JW, Cody M, et
al. Gender, kinship and caregiver burden: the case of community-dwelling
memory impaired seniors. Int J Geriatr Psychiatry. 2003;18:722-732.
12. White CL, Poissant L,
Cote-LeBlanc G, et al. Long-term caregiving after stroke: the impact on
caregivers' quality of life. J Neurosci Nurs. 2006;38(5):354-360.
13. Schulman-Green D, McCorkle R,
Curry L, et al. At the crossroads: making the transition to hospice.
Palliat Support Care. 2004;2(4):351-360.
14. Beers MH, Jones TV, Berkwits M,
et al. (eds) The Merck Manual of Health and Aging. Whitehouse Station,
NJ: Merck Research Laboratories; 2004:165-183.
15. Heath A. Long-Distance
Caregiving: A Survival Guide for Far Away Caregivers, Impact Pub, 1993. 10
Strategies for Long-Distance Caregiving. Available at:
www.webmd.com/content/pages/5/4041_130?z=4041_12. Accessed on November 20,
2006.
16. Zagaria ME. Seniors as
caregivers. US Pharm. 2004;29(3):16-25.
17. Rice DP, Fox PJ, Max W, et al.
Datawatch: the economic burden of Alzheimer's disease care. Health
Affairs. 1993;12:164-176.
18. Wilson DM. End-of-life care
preferences of Canadian senior citizens with caregiving experience. J Adv
Nurs. 2000;31:1416-1421.
19. Ansberry C. Parents devoted to a
disabled child confront old age. Wall Street Journal, January 7, 2004.
20. Fox-Grage W, Gibson MJ. Emerging
Trends and Practices in Family Caregiver Support Research Report. AARP Public
Policy Institute. March 2006. Available at:
www.aarp.org/research/longtermcare/resources/inb120_caregiver.html. Accessed
November 20, 2006.
To comment on this article, contact [email protected].











