THE QUALITY OF TEARS AND CONTACTS
By Linda Conlin, ABOC, NCLEC
Release Date: May 1, 2021
Expiration Date: February 10, 2024
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Explain dry eye causes and symptoms.
- Describe the physiological and anatomical changes that occur with dry eye.
- Describe current recommendations to manage dry eye.
- Explain contact lens fitting considerations for patients with dry eyes to increase comfort and wearing time.ar.
To Earn Continuing Education Credit:
This course has been approved for one (1) hour of Ophthalmic Level II continuing education credit by the NCLE. To earn NCLE credit, please review the questions and take the test at 2020mag.com/ce. Note: As of January 2020, no tests will be graded manually. Please call (800) 825-4696 for more information.
 You may be able to “Cry Me a River” but still
have dry eye syndrome, also known as dry eye
disease (DED). A variety of factors beyond the
quantity of tears contribute to dry eye. The doctor will evaluate the dry eye patient for tear
quality, quantity and stability. Knowing the
causes, symptoms and treatment options is
essential to increase comfort for contact lens
wear. Contact lens-induced dry eye (CLIDE) is
the leading cause of discontinued contact lens
wear. This course will review current treatment
options/technologies designed to reduce dry
eye in general and with CLIDE.
Dry eye is a common reason for eye discomfort
among contact lens wearers. Likewise, contact
lens wear is a common reason for dry eye disease.
A typical complaint heard from people who
wear contact lenses is that their contact lenses
make their eyes feel dry. Dry eye occurs with
contact lens wearers and non-wearers alike, but
people who wear contact lenses experience more
pronounced symptoms. Contact lens wearers
report they feel that their contacts start to dry out.
Dry eye poses a challenge in patients wearing
contact lenses. New treatments and contact lens
technologies allow the practitioner to keep
patients comfortable wearing contacts.
The Tear Film and Ocular Surface Society’s
Dry Eye Workshop II definition: “Dry eye is a
multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear
film and accompanied by ocular symptoms, in
which tear film instability and hyperosmolarity
(wettability), ocular surface inflammation and
damage, and neurosensory abnormalities play etiological roles.” (Nelson JD, Craig, JP, Esen
A, et al. TFOS DEWS II Report. Ocul Surf
2017; 2017 July;15(3):269-650)
You may be able to “Cry Me a River” but still
have dry eye syndrome, also known as dry eye
disease (DED). A variety of factors beyond the
quantity of tears contribute to dry eye. The doctor will evaluate the dry eye patient for tear
quality, quantity and stability. Knowing the
causes, symptoms and treatment options is
essential to increase comfort for contact lens
wear. Contact lens-induced dry eye (CLIDE) is
the leading cause of discontinued contact lens
wear. This course will review current treatment
options/technologies designed to reduce dry
eye in general and with CLIDE.
Dry eye is a common reason for eye discomfort
among contact lens wearers. Likewise, contact
lens wear is a common reason for dry eye disease.
A typical complaint heard from people who
wear contact lenses is that their contact lenses
make their eyes feel dry. Dry eye occurs with
contact lens wearers and non-wearers alike, but
people who wear contact lenses experience more
pronounced symptoms. Contact lens wearers
report they feel that their contacts start to dry out.
Dry eye poses a challenge in patients wearing
contact lenses. New treatments and contact lens
technologies allow the practitioner to keep
patients comfortable wearing contacts.
The Tear Film and Ocular Surface Society’s
Dry Eye Workshop II definition: “Dry eye is a
multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear
film and accompanied by ocular symptoms, in
which tear film instability and hyperosmolarity
(wettability), ocular surface inflammation and
damage, and neurosensory abnormalities play etiological roles.” (Nelson JD, Craig, JP, Esen
A, et al. TFOS DEWS II Report. Ocul Surf
2017; 2017 July;15(3):269-650)
DRY EYE DISEASE (DED)
Dry eye is the lack of sufficient lubrication and moisture on the eye’s surface because of decreased quality or quantity of tears. “Dry eye disease amplifies hyperosmolarity in an unforgiving cycle either directly or by inducing a cascade of inflammatory events, contributing to a loss of epithelial and goblet cells that decreases surface wettability and promotes early tear film breakup.” (Nelson JD, Craig, JP, Esen A, et al. TFOS DEWS II Report. Ocul Surf 2017; 2017 July;15(3): 269-650) Dry eye is more prevalent among smokers and women, and often occurs due to incomplete lid closure following blepharoplasty. Currently, between 16 million and 49 million Americans have dry eyes. However, this number may be three times higher. What’s more, the incidence of dry eye is increasing due to an aging population and a dramatic rise in digital device use among all age groups. When viewing digital screens, people blink at a rate of about one-third the normal blink rate, decreasing the eye’s lubrication.
SYMPTOMS AND CAUSES OF DRY EYE
Symptoms include persistent dryness, scratchiness, burning, foreign body sensation, blurred vision, light sensitivity and surprisingly, tear overproduction. Tear overproduction results in poor tear quality. The tear film has three layers (Lipid, Mucin and Aqueous) that when healthy, work in tandem to make quality tears that lubricate the eyes.
Some causes of dry eye:
• Aging: The elderly make fewer tears due to hormonal changes. Men and women can get dry eyes. But the prevalence in women is higher, especially in post-menopausal women.
• Systemic diseases:
• Rheumatoid Arthritis
• Lupus
• Thyroid disease
• Sjogren syndrome—a disorder of the immune system characterized by dry eyes, dry mouth and fatigue. It is commonly associated with rheumatoid arthritis and lupus, resulting in a decreased production of tears, saliva and sweat. It occurs more often in women over age 40 and is treated with increased water intake, eye drops and drugs. Sjogren syndrome gained national attention in the late summer of 2011 when tennis-pro Venus Williams, then 31, announced she suffered from the syndrome and its symptoms. Williams cited fatigue as the reason she withdrew from her 13th U.S. Open. Williams returned to competition and as of February 2021, at age 39, ranks 7th in the WTA. WTA Tennis. (www.wtatennis. com/search/query/Venus%20Williams)
• Eye disease/disorders:
• Blepharitis (when eyelids are swollen or inflamed—inflammation of the lid follicles blocks the production of the oily component of tears).
• Meibomian Gland Dysfunction: a study by Alghamdi et al. indicates that the first two years of contact lens wear result in both gland dropout and gland orifice obstruction, stabilizing after this point. According to this study, contact lens wear contributes to meibomian gland dropout. Meibomian glands are responsible for preventing the evaporation of the tear film. According to American Optometric Association, if MGD is not treated, a more severe form of this ocular surface disease can develop and can display symptoms that can alter the quality of life. Because MGD causes evaporative dry eye, the cornea can become desiccated and dry to a point where scar tissue can form. If MGD is chronic, it can cause the meibomian glands to atrophy. Once they are atrophied, it is very difficult to make them function normally again. MGD can develop into ocular rosacea, which can require more aggressive medical treatment.
• Ocular rosacea
• Entropion (when eyelids turn in); ectropion (eyelids turn outward).
• Dry environments such as houses with forced hot air heating and air conditioning; airplanes.
• Climate: smoke, wind or a very dry climate.
• Reduced blinking with activities such as staring at digital screens for a long time and reading.
• Post-refractive eye surgery, such as LASIK.
• Smokers have a higher prevalence of dry eye.
• Alcohol consumption can contribute to dry eye.
• Medications sometimes cause dry eye syndrome by reducing tear secretion:
• Diuretics (water pills) for high blood pressure.
• Beta-blockers for heart problems or high blood pressure.
• Allergy and cold medicines (antihistamines).
• Sleeping pills
• Heartburn medicines
• Trihexyphenidyl Parkinsons medication
• Oral contraceptives
• Anticholinergics used to treat colic or chronic bronchitis
• Tricyclic and tetracyclic antidepressants
• Neuroleptics
• Ergotamine used for acute migraine attacks
• Pain relievers - Ibuprofen
• Extended use/wear of contact lenses (CLIDE): CLIDE is the acronym for Contact Lens-Induced Dry Eye and can be used to remember the leading causes of dry eye: Climate, Drugs, Environment. Contact lens discomfort (CLD) is the most common reason why 10 to 50 percent of wearers drop out of contact lens wear within three years.
HEALTHY TEAR FILM
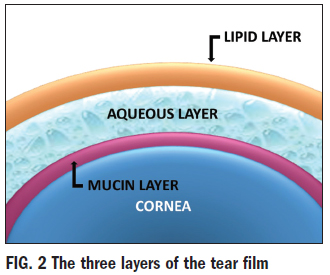 Having a healthy quality and quantity of
tears are critical factors in the management
of dry eye disease, so let’s look at the source
and composition of tears. The tear film consists of three layers: lipid, aqueous and
mucin (Fig. 2). The outer lipid layer is oily
and prevents the evaporation of tears. It is
manufactured by the meibomian glands
located on the lid margins. In the study,
“Importance of the lipid layer in human tear
film stability and evaporation,” (Optom
Vision Sci. 1997;74(1):8-13), Craig J, Tomlinson A., states that “A severely compromised
or absent lipid layer leads to evaporative dry
eye. Contact lens wear disrupts the lipid layer.”
The middle, the aqueous layer, is the largest
portion of the tear film. It supplies oxygen
to the cornea, and lubricates and protects the
ocular surface, washing away foreign materials from the conjunctiva or cornea.
The aqueous layer contains antibacterial
factors. The aqueous layer’s soluble mucin
content boosts the spread and consistency
of the layer and enhances the thickness of
the tear film. The lacrimal glands above the
outer canthus secrete the aqueous layer of the
tear film. The mucin layer is the tear film’s
inner layer and is produced by the goblet
cells in the conjunctiva, allowing for the
highest concentration of mucins at the ocular
surface. Mucins help stabilize and spread
tear film, prolonging the tear breakup time
(TBUT). This layer is vital to a stable ocular
surface since it lubricates and protects the
cornea and anchors the aqueous tear film to
the corneal epithelium. Without this layer,
tears wouldn’t adhere to the surface, making
it susceptible to damage. It’s easy to see how
poor composition or inadequate production of any layer of the tears could lead to
insufficient lubrication and moisture on the
eye’s surface. The 2013 TFOS contact lens
discomfort (CLD) reports this about low
TBUT “… a low TBUT is associated with
CLD, as is tear ferning.”
Having a healthy quality and quantity of
tears are critical factors in the management
of dry eye disease, so let’s look at the source
and composition of tears. The tear film consists of three layers: lipid, aqueous and
mucin (Fig. 2). The outer lipid layer is oily
and prevents the evaporation of tears. It is
manufactured by the meibomian glands
located on the lid margins. In the study,
“Importance of the lipid layer in human tear
film stability and evaporation,” (Optom
Vision Sci. 1997;74(1):8-13), Craig J, Tomlinson A., states that “A severely compromised
or absent lipid layer leads to evaporative dry
eye. Contact lens wear disrupts the lipid layer.”
The middle, the aqueous layer, is the largest
portion of the tear film. It supplies oxygen
to the cornea, and lubricates and protects the
ocular surface, washing away foreign materials from the conjunctiva or cornea.
The aqueous layer contains antibacterial
factors. The aqueous layer’s soluble mucin
content boosts the spread and consistency
of the layer and enhances the thickness of
the tear film. The lacrimal glands above the
outer canthus secrete the aqueous layer of the
tear film. The mucin layer is the tear film’s
inner layer and is produced by the goblet
cells in the conjunctiva, allowing for the
highest concentration of mucins at the ocular
surface. Mucins help stabilize and spread
tear film, prolonging the tear breakup time
(TBUT). This layer is vital to a stable ocular
surface since it lubricates and protects the
cornea and anchors the aqueous tear film to
the corneal epithelium. Without this layer,
tears wouldn’t adhere to the surface, making
it susceptible to damage. It’s easy to see how
poor composition or inadequate production of any layer of the tears could lead to
insufficient lubrication and moisture on the
eye’s surface. The 2013 TFOS contact lens
discomfort (CLD) reports this about low
TBUT “… a low TBUT is associated with
CLD, as is tear ferning.”
Note: Contact lens wear affects the lipid layer spread, tear film stability and tear evaporation, which contributes to contact lens discomfort (CLD). A reduction in tear film stability and impaired lipid layer function results in less lubrication and greater friction between the contact lens and the ocular surface, proliferating the cycle of CLD. A healthy tear film is crucial to ocular health, comfort and vision. Tear film destabilization caused by contact lens wear can lead to reduced comfort and wearing times, and may ultimately lead to discontinuation of wear.
DRY EYE CLASSIFICATION
The National Eye Institute states that tears are composed of a mixture of oil, water and mucus, a combination that ensures the surface of the eyes remains smooth and clear, as well as protecting the eyes from infection.
Dry eye syndrome generally occurs for one of three reasons:
• The glands of the eyes are unable to create an adequate amount of tears.
• The tears evaporate too rapidly.
• There is an imbalance in the composition of the tears.
The NEI identified two classifications of dry eye syndrome based on the type of tear deficiency: aqueous tear deficiency (ATD) and evaporative tear deficiency (ETD). Aqueous tear deficiency is an insufficiency in the aqueous or watery layer of tears and is the most common type of dry eye. Causes include lacrimal gland deficiency, lacrimal gland duct obstruction, reflex block and systemic drugs. Evaporative tear deficiency is an insufficiency of the lipid or oily tear layer, which functions to slow tear evaporation. Causes include meibomian gland dysfunction (MGD), disorders of the eyelids, low blink rate, drug side effects, vitamin A deficiency, contact lens wear and ocular surface disease such as occurs from allergies. Also, patients can suffer from a combination of both ATD and ETD. Eom HD, Jung JU, Lee KP, et al., researched tear breakup dynamics and their relation to DED treatment. NEI identified that a dot breakup pattern indicated ocular surface inflammation, and the focus should be the regeneration of corneal epithelial cells. The study also identified that a random breakup pattern indicated a destabilized tear film. (“Simplified classification of tear film breakup patterns and their clinicopathological correlations in patients with dry eye disease,” Eye Contact Lens. May 14, 2020)
TESTING
Eyecare practitioners (ECPs) commonly use two tests to classify dry eye syndrome: the Schirmer test and the Tear Break Up Time (TBUT) test. The Schirmer test evaluates the quantity of tears. A thin strip of filter paper is placed inside the lower lids of both eyes. One can perform the test without an anesthetic. However, the test is more accurate with an anesthetic because irritation from the paper may temporarily increase tear production. After five minutes, the practitioner evaluates the moisture of the eye by observing how much of the filter paper became wet through capillary action. Fifteen millimeters or more is considered normal. Nine to 14 millimeters indicates mild insufficiency. Four to 8 millimeters indicates moderate insufficiency, and less than 4 millimeters indicate a severe condition. In conjunction with the Schirmer test, applying fluorescein drops will indicate whether tears can drain through the lacrimal duct into the nose. A similar procedure is the cotton thread test. The practitioner uses a chemically treated cotton thread instead of filter paper. The thread changes color as it moistens. The practitioner then measures the length of the color change on the thread. Lengths of less than 10 millimeters indicate dryness. The advantages of the cotton thread test are that it indicates results in 15 seconds as opposed to five minutes, and it does not require anesthetic drops. The TBUT (Tear Breakup Time) test evaluates tear quality by measuring how long it takes for dry spots to appear on the cornea after a blink. The ECP applies fluorescein to the patient’s eye and then observes the tear film after a blink while the patient tries to avoid the next blink. The practitioner counts by seconds until a dry spot appears. A tear breakup time of more than 10 seconds is normal, from 5 to 10 seconds is marginal, and less than 5 seconds is low. A 2012 study by Isabelle Jabert, OD, and colleagues at the University of New South Wales, Sydney, found that increased lower lid margin sensitivity was related to more concentrated tears and meibomian gland dysfunction, which contribute to dry eye. ECPs can conduct the sensitivity test, called esthesiometry, in the office using an esthesiometer or a cotton-tipped applicator applied to the lower lid margin. The patient’s reaction to the least amount of pressure indicates sensitivity that is normal, reduced or absent. Interestingly, the study’s finding of a higher concentration of tears indicates an aqueous deficiency, while the additional finding of meibomian gland dysfunction indicates an evaporative deficiency. Patients with reduced lower lid margin sensitivity, therefore, are likely to have a combination of the two classifications of dry eye syndrome. The relationship between lid margin sensitivity and dry eye has been born out in subsequent studies.
Other diagnostic tests for dry eye include: tear film osmolarity (tests the saltiness of tears) and tear meniscus height. The tear meniscus is the thin strip of tear fluid at the upper and lower lid margins. A low or absent meniscus is an indication of dry eye.
TREATMENTS
The American Optometric Association (AOA) recommends the following:
Treatments for dry eyes should aim to restore or maintain the normal amount of tears in the eye to minimize dryness and related discomfort and to maintain eye health.
Adding tears. Mild cases of dry eyes can often be managed using over-the-counter artificial tear solutions. These can be used as often as needed to supplement natural tear production. Preservative-free artificial tear solutions are recommended because they contain fewer additives, which can further irritate the eyes. People with dry eyes that don’t respond to artificial tears alone will need to take additional steps to treat their dry eyes.
Conserving tears. Keeping natural tears in the eyes longer can reduce the symptoms of dry eyes. This can be done by blocking the tear ducts through which the tears normally drain. The tear ducts can be blocked with tiny silicone or gel-like plugs that can be removed if needed. Or a surgical procedure can permanently close the tear ducts. In either case, the goal is to keep the available tears in the eye longer to reduce problems related to dry eyes.
Increasing tear production. A doctor of optometry can prescribe eye drops that increase tear production. Taking an omega-3 fatty acid nutritional supplement may also help.
Treating the contributing eyelid or ocular surface inflammation. A doctor of optometry might recommend prescription eye drops or ointments, warm compresses and lid massage, or eyelid cleaners to help decrease inflammation around the surface of the eyes.
While there is no cure for chronic dry eye syndrome, preventive measures combined with the management of symptoms can increase contact lens comfort. ECPs can help patients manage the symptoms. When the patient is complaining of dry eye or contact lens discomfort, they should always be referred to the doctor for a comprehensive dry eye evaluation.
The AAO recommends: “A stepwise approach treatment of dry eyes generally begins with artificial teardrops, gels and ointments, cyclosporine drops (e.g., Restasis or Cequa), lifitegrast drops (e.g., Xiidra), and punctal plugs. Changing the local environment, such as using humidifiers and staying away from drafts, can also be very helpful. Other treatments include cautery of the tear drainage ducts (when plugs aren’t staying in), Lacriserts, acetylcysteine (Mucomyst) for mucous filaments and permanent partial closure of the eyelids (small lateral tarsorrhaphy). Dry eye syndrome is often a chronic condition but can usually be controlled with treatment.
“Treatment depends partly on whether it is more anterior or posterior. Generally, it includes a combination of warm compresses, eyelid scrubs, artificial tears, antibiotic drops or ointment, cyclosporine or lifitegrast, and occasionally topical steroids or oral antibiotics. Blepharitis, like dry eye syndrome, is often a chronic condition but can usually be controlled with treatment. For eyelid inflammation not responding to medical therapy, an in-office Lipiflow procedure can improve dryness symptoms by evacuating meibomian gland obstructions to improve lipid flow.”
CONTACT LENS OPTIONS
 As you recall, CLIDE also is an acronym
for Contact Lens-Induced Dry Eye. In this
condition, the presence of the contact lens
and decreased corneal sensitivity from longterm contact lens wear disrupt normal tear
film, resulting in a shorter breakup time.
While the practitioner must have special
consideration for these patients, there are a
variety of contact lens options within the
categories of rigid and soft lenses.
Rigid lenses are less susceptible to dehydration on the eye, but dry eye patients may
have a longer adjustment time due to edge
awareness. These lenses may not work well
in dry environments if the tear film is compromised. Consider corneal refractive therapy (CRT) for dry eye patients, especially
those who have worn rigid lenses. With
CRT, the patient wears rigid lenses overnight to reshape the cornea and eliminate
the need for corrective lenses. Wearing the
lenses only overnight reduces tear evaporation and the risk of drying during the day.
For severe dry eye cases, rigid scleral lenses
can become a prosthetic ocular surface. The
lens is designed with computer-assisted lathe
cut-back curves to vault the cornea. Saline in
the dome continually bathes the cornea to
provide relief.
High water content soft lenses can be
problematic for dry eye patients. The lenses
themselves may draw moisture from tears
to maintain hydration. Silicone hydrogel
lenses are a better choice because they have
high oxygen transmission but low water
content. Some silicone hydrogel lenses have
on-eye wettability. It is a surface treatment
that accommodates tear film behind the
lens and reduces the friction between the lids
and the lens for better comfort. Daily disposable lenses are another good option.
Some of the new lenses have a water and
oxygen content similar to that of the cornea.
Their surface treatment is designed to mimic
the lipid layer of the tear film. Contact lenses
with molecular imprinting are becoming
available. CooperVision Proclear lenses contain phosphorylcholine (PC) molecules that
bind with water molecules in natural tears to
create a “shield” of water around the lens. In
addition, researchers are developing daily
disposable and silicone hydrogel lenses
imprinted with an adjustable release comfort
agent. And research is underway to develop
contact lenses that improve tear fluid volume
to aid in the management of ocular diseases
like dry eye syndrome.
As you recall, CLIDE also is an acronym
for Contact Lens-Induced Dry Eye. In this
condition, the presence of the contact lens
and decreased corneal sensitivity from longterm contact lens wear disrupt normal tear
film, resulting in a shorter breakup time.
While the practitioner must have special
consideration for these patients, there are a
variety of contact lens options within the
categories of rigid and soft lenses.
Rigid lenses are less susceptible to dehydration on the eye, but dry eye patients may
have a longer adjustment time due to edge
awareness. These lenses may not work well
in dry environments if the tear film is compromised. Consider corneal refractive therapy (CRT) for dry eye patients, especially
those who have worn rigid lenses. With
CRT, the patient wears rigid lenses overnight to reshape the cornea and eliminate
the need for corrective lenses. Wearing the
lenses only overnight reduces tear evaporation and the risk of drying during the day.
For severe dry eye cases, rigid scleral lenses
can become a prosthetic ocular surface. The
lens is designed with computer-assisted lathe
cut-back curves to vault the cornea. Saline in
the dome continually bathes the cornea to
provide relief.
High water content soft lenses can be
problematic for dry eye patients. The lenses
themselves may draw moisture from tears
to maintain hydration. Silicone hydrogel
lenses are a better choice because they have
high oxygen transmission but low water
content. Some silicone hydrogel lenses have
on-eye wettability. It is a surface treatment
that accommodates tear film behind the
lens and reduces the friction between the lids
and the lens for better comfort. Daily disposable lenses are another good option.
Some of the new lenses have a water and
oxygen content similar to that of the cornea.
Their surface treatment is designed to mimic
the lipid layer of the tear film. Contact lenses
with molecular imprinting are becoming
available. CooperVision Proclear lenses contain phosphorylcholine (PC) molecules that
bind with water molecules in natural tears to
create a “shield” of water around the lens. In
addition, researchers are developing daily
disposable and silicone hydrogel lenses
imprinted with an adjustable release comfort
agent. And research is underway to develop
contact lenses that improve tear fluid volume
to aid in the management of ocular diseases
like dry eye syndrome.
A recent study successfully demonstrates the potential of HA-GO loaded contact lenses to improve tear fluid volume to manage various ocular diseases like dry eye syndrome. (Chao Huang, Xin Zhang, Yanchun Li & Xiaolan Yang (2021) Hyaluronic acid and graphene oxide loaded silicone contact lens for corneal epithelial healing, Journal of Biomaterials Science, Polymer Edition, 32:3, 372384, DOI:10.1080/09205063.2020.1836926).
Contact lens solutions are an important consideration for dry eye patients. Some solutions work better with certain contact lens materials than others. Check with the lens manufacturer for solution recommendations.
Advise patients against using generic solutions, which can vary from purchase to purchase. Because proteins build up more quickly on lenses for dry eye patients, recommend rub and rinse solutions to provide better cleaning. Intolerance to preservatives in solutions can result in dry eyes. Peroxide disinfection systems eliminate preservative intolerance problems and the variations common in generics but make sure the patient knows how to use them.
Dry eye patients should only be fit in contact lenses after symptoms subside. Complete treatment with topical steroids before contact lens fitting. Be sure that the base curve, diameter and lens material allow for appropriate tear exchange. Patients should avoid overnight wear, and patients who wear their lenses more than 10 hours per day should make time to remove, clean and reinsert the lenses at some point. Recommend a frequent lens replacement schedule to reduce the risk of irritation from protein buildup, as well as more frequent follow-up visits.
CONCLUSION
Dry eye is a prevalent condition and is on the rise. More of us will suffer from dry eyes as Baby Boomers age, and young and old spend increasingly more time staring at our digital device screens. Dry eye symptoms complicate contact lens wear and lead to a high rate of discontinuance. Early introduction of dry eye management is recommended for contact lens wearers since maintaining a healthy tear film is vital to contact lens comfort. Evaluating the contact lens wearers’ quality and quantity of the tear film and the healthy functioning of the meibomian glands is a vital aspect of managing CLIDE. Contact lens materials are improving, as are topical medications and surface treatment solutions, and artificial tears to help dry eye patients achieve comfortable contact lens wear.



