Taming the Wild Wavefront – Part 2
Improving Eyewear Satisfaction With a Refined Rx and Customized Lenses
By Mark Mattison-Shupnick, ABOM
Release Date: January, 2014
Expiration Date: December 13, 2018
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Learn why patients may not be happy with their glasses in all types of lighting conditions.
- Understand how high-order aberrations affect vision.
- Learn how new instruments and technologies can provide added precision to the prescription, the measurements required and the way lenses are fabricated to deliver eyewear unlike any previously delivered.
Faculty/Editorial Board:
 Mark Mattison-Shupnick, ABOM, is currently director of education for Jobson Medical Information LLC, has more than 40 years of experience as an optician, was senior staff member of SOLA International and is a frequent lecturer and trainer.
Mark Mattison-Shupnick, ABOM, is currently director of education for Jobson Medical Information LLC, has more than 40 years of experience as an optician, was senior staff member of SOLA International and is a frequent lecturer and trainer.
Credit Statement:
This course is approved for one (1) hour of CE credit by the American Board of Opticianry (ABO). Course STWJH524-2
Support:
This course is supported by an educational grant from CARL ZEISS VISION.
As we learned in Part 1, low-order aberrations (prism, defocus and astigmatism) have been corrected, but with compromise, for decades. While traditional lenses provided an adequate prescription solution, for many the optics were less than adequate in the periphery or when the lenses had significant pantoscopic tilt or wrap. The effects of base curve choice and position of wear degraded the edge-to-edge visual clarity of the lenses. These compromises were unavoidable using the technology of the time. However, the combination of real-time optical design and free-form lens manufacturing now allows for the optimization or customization of lenses for virtually all prescriptions and positions of wear. This provides a better eyewear solution than ever before.
Eyes, however, are subject to wavefront aberrations beyond prism, defocus and astigmatism. High-order aberrations (HOAs) of the eye affect vision in large pupils differently than when the pupil is small; in bright versus low-light conditions and for many people, the impact on night vision is significant. High-order aberrations are also much more challenging from a vision-correction standpoint. A standard refraction won't detect them, and spectacle lenses can't correct them the way they correct low-order aberrations. However, new technology allows us to make spectacle lenses that can significantly improve visual quality over a range of viewing conditions, including nighttime, for many people by at least taking high-order aberrations into account when determining the sphere and cylinder corrections. Here's how.
PUPIL SIZE, AVAILABLE LIGHT AND BLUR
The pupil of the human eye varies from roughly 2 mm in diameter in bright daylight to roughly 8 mm in diameter in total darkness (Fig. 1). It's during mesopic (intermediate lighting conditions using rods and cones) and scotopic vision (dark lighting using only rods) that the higher-order aberrations come out to play.
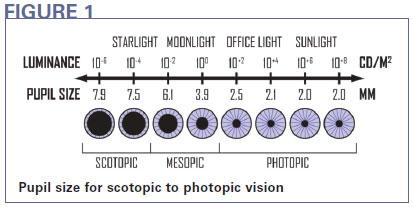
Low-order aberrations, including the familiar spherical defocus and astigmatism that are responsible for the basic "refractive errors" of the eye, produce image blur that increases with both pupil size and refractive error. High-order aberrations also reduce image quality, especially when the pupil size is large, by further diffusing the image focus, reducing image contrast or by causing "halos" and similar effects around bright lights at night.
Some refer to high-order aberrations as a kind of "image noise," which can be defined as "reduced image quality created by ocular and optical distortions present within the vision correction system. For the average person, image noise represents approximately 17 percent to 20 percent of the total refractive error." (Catania L., "Wavefront diagnosis: The Future of Vision and Eyecare." Presentation at 107th Annual Optometric Association Congress 2004)
Image noise is dramatically influenced by pupil size; when corrected, the reduction is perceived by the patient as improved visual clarity. Current clinical references indicate that up to 20 percent improvement in image clarity may be achieved by eliminating excess image noise from a system.
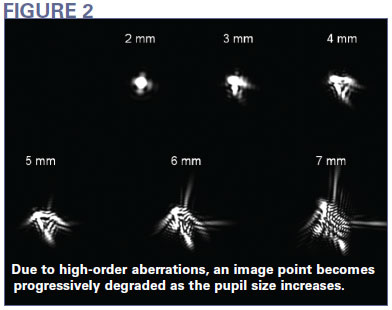
The effects of increased pupil size can be seen in Fig. 2. The point of light for the 2 mm pupil is fairly compact and concentrated, whereas the point of light for the 7 mm pupil has become distorted with no clear definition due to the presence of high-order aberrations.
SIGNIFICANCE OF HOAs
What constitutes an "ideal vision correction" is dependent on the viewing conditions, including light level, working distance and nature of the object of regard. The standard Rx is ideal only for the specific conditions of the exam room. The subjective refraction generally uses a brightly illuminated, high-contrast visual acuity chart, sometimes with normal room lighting. This causes the pupil of the eye to remain relatively small, which means that high-order aberrations won't be noticeable to the patient.
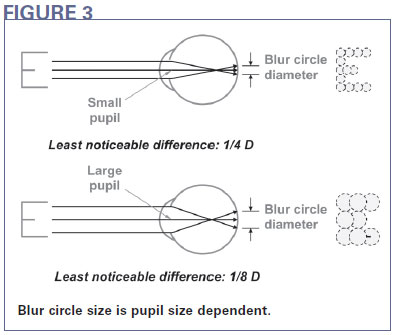
Why is that? The answer is surprisingly simple. The rays of light that are most affected by HOAs are the marginal rays that enter the eye away from the optical axis. They don't affect vision as much under normal lighting conditions because the small pupil size prevents them from entering the eye. The only rays that enter a small pupil are those close to the optical axis, or paraxial (Fig. 3). A larger pupil allows these marginal rays to enter the eye, where HOAs prevent them from intersecting at the paraxial focus. As a result, the point of best focus is no longer on the retina. This creates phenomena such as "night myopia" and "irregular astigmatism."
Depending on the extent of the patient's HOAs, the ideal prescription power can differ significantly with pupil size. For normal eyes, the difference in sphere and cylinder powers between a 3 mm and a 7 mm pupil averages roughly +0.25D. For eyes with significant HOAs or irregular corneas, the difference averages roughly +1.00D.
ERRORS IN REFRACTION
Two factors can influence the effectiveness of a standard refraction in low-light conditions. One is that the presence of HOAs creates a difference in the ideal correction between small and large pupil sizes, as discussed above. The second is the patient's blur tolerance, which is higher at small pupil sizes than it is at large sizes. These two factors can combine to create a difference between the prescription determined in the subjective refraction and the patient's needs in lower light.
During the refraction, blur measured is the result of the size of the blur circles determined by the extent of the refractive error—how far the point of best focus is from the retina. If the point of best focus were closer to the retina, obviously the blur circle would be smaller. By blocking out the rays that deviate most, a small pupil makes the blur circle smaller. For a small pupil size, "the least noticeable difference" in power is often one-quarter (0.25D) diopter, which is why a standard phoropter has 0.25-D clicks. But if you double the pupil size, you double the size of the blur circles. This makes it easier to notice smaller differences in power. The least noticeable difference is now one-eighth (0.125D) diopter.
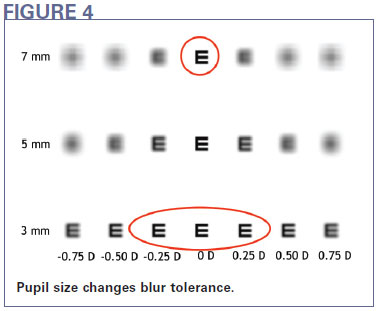
This means that a given patient might not notice the difference among three clicks of the phoropter when his or her pupil is small (Fig. 4). In the daytime, that patient might be perfectly happy with any of these powers. However, at large pupil size, only the one in the middle is optimum. Given that traditional lens surfacing is done to a tolerance of 0.13D, the night vision correction could be off by as much as 0.38 diopters. Further, at large pupil sizes, the effects of high-order aberrations can influence the refractive error significantly, resulting in further errors from the ideal vision correction.
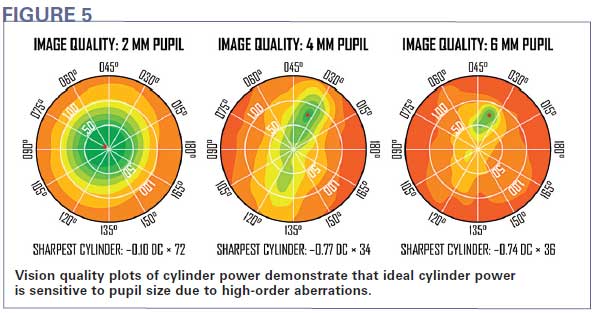
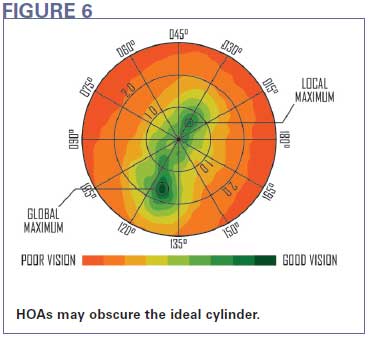
Finding the cylinder correction at a small pupil size can also be challenging. As with spherical correction, the eye is more tolerant to errors from the ideal cylinder correction at small pupil sizes, and high-order aberrations can influence the refractive findings at larger pupil sizes, so finding the best correction becomes more critical for a larger pupil. In Fig. 5, the cylinder power varies from an essentially spherical prescription (only 0.10D of cylinder power) at a small pupil size to over 0.75D of cylinder power at larger pupil sizes. In addition, HOAs may result in multiple cylinder power and axis combinations that produce good results. As seen in Fig. 6, a subjective refraction using the cross-cylinder technique may find one of these "good" corrections ("local maximum"), but miss the ideal correction needed for more demanding low-light conditions ("global maximum").
WHAT WE CAN'T DO
Even if the high-order aberrations were precisely mapped in the exam, spectacle lenses couldn't correct them. Why not?
Correcting any order of aberrations introduces lower-order aberrations when the eye moves away from the center of the correction. For second-order sphere and cylinder power, first-order prism is introduced when the eye moves (the basis of Prentice's rule). For third- and higher-order wavefront corrections, second-order aberrations (defocus and astigmatism) are introduced when the eye looks away from the center of the lens. The second-order aberrations induced by eye movement will actually produce more blur away from the center of the lens than was actually eliminated in the first place by the high-order correction at the center of the lens.
THE CAN-DO PRESCRIPTION
Enough about what we can't do; what CAN we do? There is evidence that patients prefer a prescription that balances the needs of small-pupil and large-pupil vision over one that is optimized for only one pupil size. (Cheng X., Bradley A. and Thibos L. "Predicting Subjective Judgment of Best Focus with Objective Image Quality Metrics." J Vis, 2004; Vol. 4, No. 4)
How to create such a balanced prescription? First of all, the subjective refraction is not outdated or unnecessary. It just can't tell us how HOAs are affecting the patient's vision under different viewing conditions. Using aberrometry, we can measure all of the wavefront aberrations of the patient's eyes to characterize more accurately the refractive status of each eye. And while we can't actually create a lens that corrects all of these aberrations, we can at least refine the prescription to account for the vision needs of a large pupil as well as a small one.
Unique to Carl Zeiss Vision is i.Scription, a technology designed to determine the optimal correction that balances the patient's vision needs over different viewing conditions, including low-contrast and low-light vision. i.Scription technology combines wavefront analysis of the eye over a range of viewing conditions, an algorithm that uses this data to refine the manifest refraction and digital lens production to deliver this more precise vision solution.
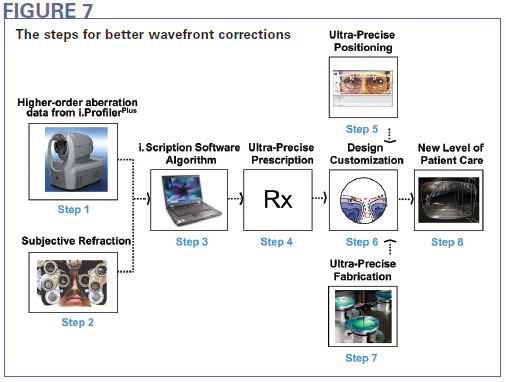
The process begins with i.ProfilerPlus, a combination wavefront aberrometer, autorefractor and corneal topographer. The i.ProfilerPlus measures the HOAs in each eye (Step 1). Using a proprietary algorithm that analyzes all of the wavefront aberrations of the eye, the i.Scription software calculates the combination of sphere power and cylinder power that maximizes the depth of focus for a medium pupil size in order to best balance the effects of aberrations at small and large pupil sizes over a range of viewing distances. However, there are some aspects of a subjective refraction that an autorefraction can never replicate. These include the patient's individual way of defining visual clarity, controlling the accommodation and binocular balancing (Step 2). Therefore, using a proprietary algorithm, the data from the aberrometer and the subjective are combined to produce the ideal wavefront-guided refraction (Step 3). The resulting prescription will typically differ slightly from the subjective findings, and since wavefront refraction is not limited to the increments of trial lenses, will be specified to a precision of 0.01 diopters (Step 4). Using digital measurements, lens design customization software and ultra-precise digital manufacturing techniques (Steps 5, 6 and 7), the final lens produced can deliver a new level of patient care.
BENEFITS
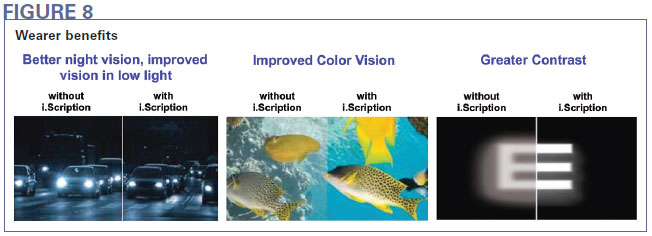
Eyewear that relies on a wavefront-guided prescription can often address a patient's complaints about night vision by reducing visual noise with a vision correction that works better in low-light viewing conditions. But these visual benefits are not restricted to nighttime vision. Many wearers also notice enhanced color perception and sharper vision during the day. Combining this with the prescription and position-of-wear customization discussed in Part 1, we can create a superior visual experience in all viewing conditions.
A UC Berkeley clinical study of 30 subjects compared wavefront-guided single vision lenses to conventional single vision lenses in a randomized, double-masked, crossover wearer trial. Performance was measured using subjective and objective tests. The results showed that subjects with low to moderate prescription powers preferred wavefront-guided lenses more often for distance vision, active vision, sharpness, changing focus and overall vision. Subjects preferred wavefront-guided lenses more often for night vision, vividness of colors and having less glare. Wavefront-guided lenses performed better than conventional spectacle lenses in measures of low-contrast and mesopic visual acuity by approximately half a line of acuity (Meister D. and Thibos L. "i.Scription by ZEISS: Setting the New Standard of Vision Correction." Carl Zeiss Vision, 2009).
In a like German study of 159 wearers, 80 percent reported better visual comfort, 74 percent saw better at night and in low-contrast situations, over 66 percent reported clearer, sharper vision and 60 percent saw colors more intensely. (i.Scription wearer trial conducted by an independent optician with 159 of his customers in Germany.)
AN IMPORTANT PATIENT OPPORTUNITY
Inevitably, we face the question of how to explain the benefits of new, more advanced lens technology to patients who know very little about lenses, and who can't experience the benefits you're describing until after they've committed to buying the eyewear. As usual, patient education is the key. Patients need to know that you are going the extra mile to understand their visual situation more precisely, which allows you to create a better, more personalized, visual experience. Most patients won't have been measured with an i.Profiler or an advanced centration device before, so already they'll perceive that there's something different going on at your practice. Make sure they understand why and what visual benefits could result.
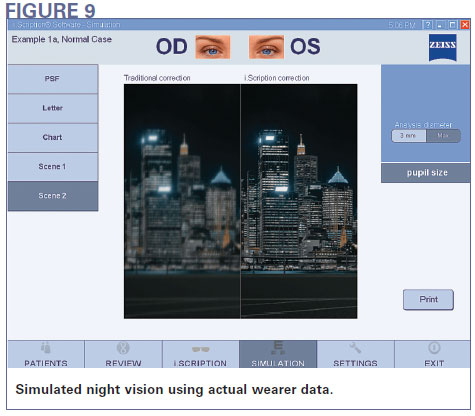
The i.Scription software is designed to help you with this process. Using patient-friendly graphics, you can show them a "map" of the HOAs in their eyes and the magnitude of those aberrations compared to population averages. Then you can show them the difference that i.Scription can make to their vision specifically: using the patient's actual results, the software can simulate the difference that the patient will experience with i.Scription versus the standard prescription.
Depending on the particular lenses and process you're using, your approach can result in any or all of the following: better distance, mid-range and near vision, improved sports vision, increased brightness of objects and the environment, more vivid color perception and increased sharpness of objects viewed. Peripheral vision can be clearer, depth perception improved and it can take less time to get used to the new lenses. Overall: more visual comfort at all distances. In fact, it becomes easier and quicker to change focus, especially in night vision. Vision can be more natural than ever before.
CONCLUSION
Today you face more competitive challenges than ever before, but you also have more tools to make your approach to vision care stand out from the rest. By continuing to add more precision to the way the prescription is defined, the lens surface is designed and the lenses are manufactured—in short, by reducing or eliminating more wavefront errors, you can improve their visual experience in a way that eyeglass lenses haven't achieved before.
By taming that wild wavefront, from prescription to lens form, you create an opportunity to elevate the patient experience, differentiate the practice, increase capture rate and patient retention, while generating increased revenue and profit potential.



