"Eyes Right!"
An Overview of Prism Use in Eyewear
By David Lineaweaver, ABOC
Release Date: February, 2018
Expiration Date: December 19, 2022
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Understand the basic optical principals of prism.
- Learn the typical use of prescription prism in eyewear: diplopia/fixation disparity correction.
- Know the function of prisms in visual field loss.
- Understand applications for yoked prism.
Faculty/Editorial Board:
David Lineaweaver, ABOC, CLVT, currently works as an ophthalmology health aid and technician at the Fort Harrison, Mont., Veterans Administration Eye Clinic. Lineaweaver's approach to optics is practical, and that serves the low vision community especially well as a Certified Low Vision Therapist.
Credit Statement:
This course is approved for one (1) hour of CE credit by the American Board of Opticianry (ABO). Technical Level II Course STWJH685-2.
“Eyes right” is a military command, given during parades and troop inspections. The troops marching will briskly snap their heads and attention to the right upon this command. A general or other high-ranking dignitary is on the right, so the troop’s focus is on them as they march by. How else might that dignitary have been seen? One could have fit prism eyewear (with a base in which direction?) to allow objects to the right to be seen with eyes straight ahead. While that’s a bit far-fetched, and we won’t march in a parade during this course, we will take a look at the various purposes for prism in eyewear.
We commonly see prism noted on eyeglass prescriptions in rectangular coordinates, as base in or out or base up and down. It may also be prescribed in a yoked fashion; base-up (both lenses), base-down (both lenses), base right or base left. In rectangular or coordinates, prism orientation is always documented in terms of the direction of the base. It is never referenced in terms of the direction of the apex.
WHAT IS A PRISM AND WHAT DOES IT DO ANYWAY?
In its basic form, a prism is simply a triangular wedge of optical material (glass, plastic, etc). The base of the prism (or hypotenuse for those who think in geometry terms) is the thickest part, and the apex is the point, opposite the base on an equilateral triangle or prism. Any leg can be designated as the base, and the opposite point will be the apex, but that is a little outside of our topic. A prism that is positioned with its base down on a table will naturally have its apex up. When a light bundle is applied, this demonstrates two constants with prisms: 1. Light is always bent toward the base of the prism, and 2. Image is always displaced toward the apex of the prism.
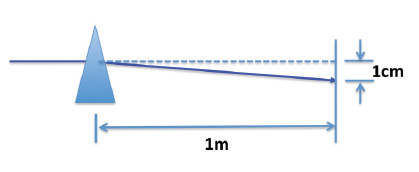
The amount of displacement is measured in prism diopters where 1 diopter prism will shift an image 1 cm at a distance of 1 meter:
Light is not bent toward the base as a single beam. It is dispersed into its component colors, like a rainbow, according to its component wavelengths. This is commonly known as dispersion. The chromatic spread is the result of the refractive index and the inherent optical characteristics of the lens material and magnitude of the prism. The resulting chromatic aberration is a consideration when selecting a material for a lens or prism, but will not be explored in depth in this course.
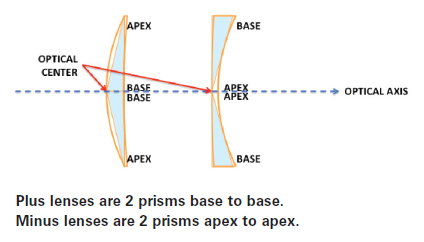
Lenses can be thought of in terms of prisms. A plus lens can be thought of as two prisms, placed base to base. A minus lens can be thought of as two prisms, placed apex to apex. The optical center, where a perpendicular beam of light passes through unrefracted, is where the two bases meet for the plus lens and where the two apexes meet for the minus lens. In basic opticianry, we learned that the optical centers of each lens should be directly in front of the corresponding pupil center, when no prism is desired. Sometimes the optical centers of the lenses can be deliberately displaced to create prescribed prism. (This can be calculated through the Prentice formula, though a detailed discussion on this is beyond the scope of this course.) Prism can be induced by decentering lenses or also be ground into lenses when creating a prescription from a semi-finished lens blank.
USING PRISM IN EYEGLASSES TO SOLVE PROBLEMS
The most common use of prism in eyewear is to correct diplopia, also known as double vision. In diplopia, the eyes can be thought of as being out of alignment with each other, with the image being projected on different points on the retina of each eye. This can be vertical, horizontal or a combination of both. Using prism aligns the images even when the eyes don’t align correctly.
Amazingly, the images don’t have to hit the exact same spot on each retina to achieve single vision. There is a buffer zone referred to as Panum’s Area, which can be thought of as concentric circles, starting at the fovea. As long as an image is projected within Panum’s Area diplopia is avoided.
Of course smaller targets are viewed in the smaller circles, closer to the fovea and are more subject to diplopia than larger targets. The misalignment may be visually obvious to an observer, or the eye may appear aligned, and the “misalignment” is functional. The prism takes the incoming image and shifts it to “where the eye is really pointing,” with the base being in the opposite direction of the deviation. This is generally accomplished with the prescribed prism amount being split between the two eyes, as this will render a more cosmetically balanced appearance in the lenses. However, the prism correction can of course be applied to just one eye instead.
Correction for horizontal diplopia may be further described as:
Esophoria or esotropia: An inward (toward the nose) turned eye or inward “seeing” eye. Base-out prism is used to correct for this and can be all in one eye or split between the two eyes. If the prism is split between both eyes, the orientation for the prism will still be base-out for both eyes. An example of “eso” correction in a prescription is:
OD: -1.00 DS Prism: 1.50 Base-out
OS: -1.25 DS Prism: 1.50 Base-out
Add: +2.25
Exophoria or exotropia: An outward (toward the ear) turned eye or outward “seeing” eye. Base-in prism is used to correct for this and can be all in one eye or split between the two eyes. If split between both eyes, the orientation for the prism will still be base-in, both eyes. An example of “exo” correction in a prescription is:
OD: +1.00 DS Prism: 1.20 Base-in
OS: +2.25 +0.75x 180 Prism: 2.50 Base-in
Base-in prism is also sometimes used to correct for convergence insufficiency. Base-in prism effectively “brings” the image out to the eyes, that won’t converge sufficiently, for reading or near work.
Correction for vertical diplopia may be further described as:
Hyperphoria/hypertropia (vertical diplopia): A higher positioned or higher “seeing” eye. Correction for hyperphoria/hypertropia may be accomplished by placing the full amount of base-down prism over the eye that appears higher or “sees” higher (hyperphoria or hypertropia) or by placing half of the prism amount base-down over the “higher” eye and half the prism amount base-up over the other eye. The following examples show two ways of documenting the desired prism, which may be filled either way, unless specified otherwise, by the prescribing provider. Full amount of prism over deviated eye:
OD -1.50-0.75 X 093 Prism: 4.0 Base-up
OS -2.00-0.75X 090
Prism split between both lenses:
OD -1.50-0.75X 093 Prism: 2.0 Base-up
OS -2.00-0.75X 090 Prism: 2.0 Base-down
The higher eye is always referenced as hyperphoric or hypertropic. The term hypophoria or hypotropia is never used.
Care must be taken in selecting frame size, shape and lens material, for prescriptions with base-in prism, as the base portion of the prismatic lens is on the nasal side and can make nosepad adjustment difficult or impossible (depending on refractive correction and prism amount).
Try keeping frame sizes moderate and symmetrical, and use high-index materials as needed. These keep the thickness of the base side of the lens manageable. Rolling the edge may also be helpful. This ensures that there is clearance for nosepad adjustment. The rolled edge can be highly polished for cosmesis, but I prefer the more subdued “satin” polish to avoid unwanted reflections. As always, a high quality anti-reflective coating is very highly recommended to enhance the overall appearance and performance of the eyewear.
Slab-off prism is designed to offset the vertical prismatic imbalance that occurs when people shift their view from the distance portion to the near add of their multifocal lenses. This vertical imbalance only needs to be compensated for when the there is a significant refractive difference between each eye, causing the patient symptomatic problems. Some people can tolerate much more imbalance than others, without experiencing symptoms; therefore, the term significant refractive difference is somewhat subjective.
In slab-off, base-up prism is placed in the lower portion of the most minus lens or the least plus lens. Reverse slab-off prism is an alternate way of relieving vertical imbalance, by placing base-down prism in the lower portion of the most plus or least minus lens. There is an excellent article in the February 2014 edition of 20/20 that goes in to more detail about slab-off prism.
The topics of prism to correct for diplopia and the various pathologies that cause it are varied. There is significant literature available to those who wish to pursue more detail than is covered here.
 Prism can also be used in treating visual field loss, as it can shift an image from a blind area into an area of seeing. The base of the prism is positioned in the blind area, which shifts the image toward the apex and into the seeing area.
Prism can also be used in treating visual field loss, as it can shift an image from a blind area into an area of seeing. The base of the prism is positioned in the blind area, which shifts the image toward the apex and into the seeing area.
A 2.0 diopter prism shifts an image approximately 1.0 degree.
Visual field loss can be treated by two different, but complementary ways: scanning for awareness and awareness devices.
Scanning for awareness: Simply turning your head toward the blind area, to view things that you couldn’t, prior to turning your head. The idea is that you are aware of the blind area and are making a conscious effort to view and be aware of things in that area. Scanning often becomes an unconscious, “second nature” action over time, if the visual field loss is long-standing or permanent. If the patient has developed effective scanning techniques and is functioning well in everyday activities, the adverse effects of visual field loss can be considered overcome; not resolved, as the visual field loss is still present, but overcome in the sense that the loss has been compensated for.
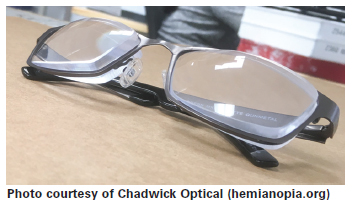
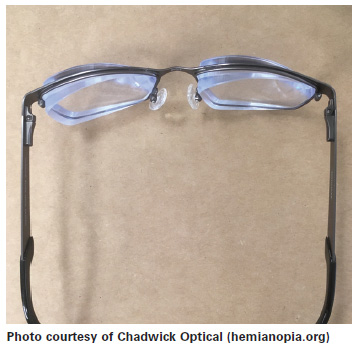
Awareness device: Prism may also be used as an “awareness” device, when it is positioned outside of the visual axis (outside of the pupil margin), with the base oriented toward the non-seeing area. This is often used for people that have homogenous hemianopia (missing half of the visual field in each eye), after suffering a stroke. The patient can view “normally” in a straight ahead fashion, then look toward the prism to gain visual access to the missing visual field, for awareness purposes. The patient can then turn his head toward the blind area, if he wishes to see something in that area more clearly.
 Visual neglect: In the case of visual neglect, the patient is not aware of any missing visual field and makes no conscious effort to compensate for it; truly a situation of “out of sight, out of mind.” This is often evidenced by patients bumping into people, or tripping over things that are on their blind side. Unfortunately, this has been a cause for many vehicle accidents as well. The person with visual neglect does not just fall into scanning, but must be reminded continually to scan. Vision therapy or occupational therapy is often recommended to develop and reinforce scanning techniques and habit. Sometimes prism can help create awareness of the blind area and resolve visual neglect.
Visual neglect: In the case of visual neglect, the patient is not aware of any missing visual field and makes no conscious effort to compensate for it; truly a situation of “out of sight, out of mind.” This is often evidenced by patients bumping into people, or tripping over things that are on their blind side. Unfortunately, this has been a cause for many vehicle accidents as well. The person with visual neglect does not just fall into scanning, but must be reminded continually to scan. Vision therapy or occupational therapy is often recommended to develop and reinforce scanning techniques and habit. Sometimes prism can help create awareness of the blind area and resolve visual neglect.
The amount of missing visual field that can be shifted into view increases as prism power increases. (Remember—a 2.0 diopter prism shifts an image approximately 1.0 degree.) However, larger prisms bring a more abrupt image jump and can take longer to get used to. Several prism powers may be trialed until the “best overall” prism power is selected. Prism positioned like this can be thought of like side mirrors on a car; used for spotchecking, but not for full time viewing. This prism “awareness device” is often used in just one lens, though it can be used in both.
For example, a patient with left visual field loss in both eyes may be prescribed a baseout prism for just the left eye, (usually placed just temporal to the pupil). He or she may also be prescribed base-in prism for the right eye (usually placed just to the nasal side of the pupil) and base-out prism for the left eye, as mentioned above. (This is yoked prism and would be specifically referred to as base-left prism.) Using prism over both eyes as an awareness device can be tricky, as it will be very important that both eyes get into the prism at the same time. This is to avoid diplopia and other visual disturbances.
Fresnel Prisms are commonly used to facilitate visual field awareness, as they are much thinner and lighter than their ground-in counterparts. Fresnel prisms are typically formed by a series of small prisms molded into thin plastic sheets, a prism ridge side across one surface, and smooth and flat on the other. This makes them very versatile, as they can easily be cut into various shapes and positioned and repositioned on spectacle lens(es) as often as necessary, right in the clinic.
 Success with prism as an awareness device is very subjective. Sometimes it just doesn’t work. Sometimes people will effectively use visual field awareness prism on a permanent basis… that’s success! Other times, people find them useful for a while and then say, “They quit working.” What that usually means is that the prism awareness device helped them develop effective scanning techniques, and they no longer need that prism to prompt scanning; that’s success too!
Success with prism as an awareness device is very subjective. Sometimes it just doesn’t work. Sometimes people will effectively use visual field awareness prism on a permanent basis… that’s success! Other times, people find them useful for a while and then say, “They quit working.” What that usually means is that the prism awareness device helped them develop effective scanning techniques, and they no longer need that prism to prompt scanning; that’s success too!
In this second scenario, the prism can be thought of as “training wheels” that helped get to the end goal of effective scanning. The training wheels process can be in the form of structured clinical therapy, or the patient can work this process on their own, with initial guidance from a qualified clinician.
In some cases, the visual field loss is temporary, and the awareness treatment is temporary as well. Sometimes the prism power can be progressively decreased as visual field is restored or scanning becomes more effective.
VISUAL MIDLINE SHIFT
Now we come to a less common and sometimes controversial condition known as Visual Midline Shift. The Neuro Optometric Rehabilitation Association (NORA) describes VMS as follows: “Visual Midline Shift results from dysfunction of the ambient visual process. It is caused by distortions of the spatial system causing the individual to misperceive their position in their spatial environment. This causes a shift in their perceived visual midline. This will frequently cause the person to lean to one side, forward and/or backward. It frequently can occur in conjunction with individuals that have had hemiparesis (paralysis to one side following TBI or CVA).” TBI is the acronym for Traumatic Brain Injury and CVA for Cerebral Vascular Accident, more commonly referred to as stroke.
The ambient visual process, mentioned above, goes beyond visual acuity. It is the process that gives a person a sense of “where they are” and “where everything else in the world is.” When this process gets disrupted, it can adversely impact a person’s ability to maintain balance, walk and do other various tasks as their perception of midline, what’s directly in front of them, has been skewed or offset. In an attempt to “re-center” their visual and physical frame of reference, people with VMS will often turn their heads and/or their bodies to what they now perceive as their “center” or what is directly in front of them… though this is not accurate. Most people who experience visual field loss do not develop VMS. However, VMS may be present in the absence of any observable compensatory head or body postures. This is where keen, detail-oriented evaluation, by a skilled clinician is paramount, as it can easily be misdiagnosed or overlooked. Treating this condition often leads to the junction where optometry, vision therapy, occupational therapy and physical therapy converge. And since glasses are sometimes prescribed, opticianry plays a role as well.
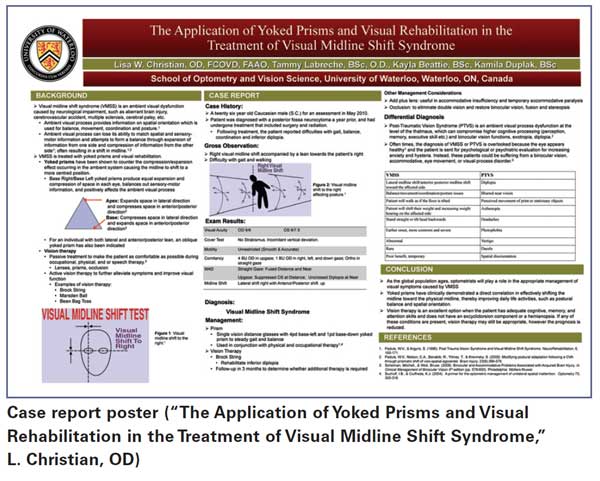
Yoked prism can be used to treat VMS. Again, this may be a permanent or indefinitely ongoing. This may also be like the training wheels mentioned earlier, with the end goal being an accurate sense of midline, without the use of yoked-prism glasses. For example, a patient may be prescribed glasses, with base-left prism (base–in OD and base-out OS) if the perceived midline and/or posture have been shifted to the right (in an attempt to re-center). The base-left prism will shift the visual center back toward the left, with the hope of restoring a more accurate visual and postural sense of midline. Remember, the base of both prisms are toward the patient’s left side and are working together to bring the missing visual field from the left into view or awareness.
The prism must be yoked, in the treatment of VMS, as use of prism in only one eye would cause diplopia. Yoked prism will take the form of one eye base-in and one eye base-out (which eye will depend on whether it is designated as base-left or base-right). This can be a confusing concept; the prisms are considered yoked if their bases are both positioned in the same direction in terms of right or left; not both being indicated as base-in or base-out, as is the case when correcting for horizontal diplopia. In addition to horizontally yoked prism, vertically yoked prism (base-up both eyes or base-down prism both eyes) may be used to treat VMS and related posture issues as well. Below are examples of how yoked prism is noted in prescriptions:
Horizontally yoked prism:
OD: -1.00-0.50 X 090 Prism: 5.0 Base-in
OS: -0.75 DS Prism: 5.0 Base-out
Vertically yoked prism:
OD: +1.50-2.00X 180 Prism: 2.0 Base-up
OS: +1.00-0.75X 165 Prism: 2.0 Base-up
Determining the amount of yoked prism needed to shift the midline to the desired position is somewhat subjective; there isn’t an exact formula; nor is there a oneto-one correlation between degrees of visual field loss in an area and the degrees of midline shift in the opposite direction. Often the midline shift is only a few degrees, even though the area of visual field loss may be much larger. For example, a patient with a right homogenous hemianopia, who has essentially lost the right side of their vision, may only shift their head and/or body position five degrees to the right, in an attempt to recenter. It is generally recommended to trial various prism strengths to see what best restores a proper sense of midline. However, it must be kept in mind that VMS is not just a visual condition, but also a neurological condition, so yoked prism may not be a silver bullet that will yield instant results. Various modalities of therapy may be indicated over a period of time. An important principal to remember when working with prism as an awareness device for visual field loss or as a “shifting” device for VMS is: There is no optical way to gain more overall visual field with prism, just the ability to redistribute it.
OTHER USES FOR YOKED PRISM
Reading glasses: One provider reports success in using yoked base–down prism in reading glasses for people with inferior visual field loss. This allows those people to read with a more normal head/eye position. This “brings” the text up instead of having to tip the headway down, in an uncomfortable way, to access the text. The provider reported that about 50 percent of the patients liked this, and there was almost immediate acceptance or rejection of the prism. Prism was usually between 5 to 10 diopters.
Prism thinning: Prism thinning is a procedure using yoked base-down prism in progressive lenses, to create a more cosmetically “balanced” looking lens (not thicker on the top and thinner on the bottom, due to the add power) and ensure that the bottom portion of the lens won’t be too thin after edging and support a bevel for good lens retention. Prism thinning is commonly done in powers up to
3.0 prism diopters, with rare visual complaints or adaption issues.
Null point: People who suffer from the constant oscillating eye movements of nystagmus usually find a null point. This is a head position that stops or brings the nystagmus movements to a minimum. Sometimes the null point is not a very comfortable head position. Yoked prism can be used to allow the patient to achieve a null point that is more comfortable.
Cosmesis: It can be more challenging to make eyewear with base-left or base-right prism, appear to have a “balanced” or symmetrical appearance, than eyewear with vertical or base-in or base-out prism. Just by design, it has a very nonsymmetrical appearance. Common “good practice” opticianry can mediate much of that, with the first order of business being to manage patient expectations.
- It is important that the patient knows that a completely symmetrical appearance between the lenses is impossible with prism in a base-left or base-right direction.
- Next, the frame choice should be kept to a moderate size, with the shape being fairly symmetrical (forget large aviator frames). Sometimes a “large gauge” plastic frame can somewhat mask the protruding edges of the lens, where the base is oriented.
- High-index lens materials can help reduce the thickness overall.
- Rolling the edges of the lenses, especially at the thickest part, can also help minimize the “out of balance” appearance. I generally prefer no edge polish or a duller “satin” polish to avoid unwanted reflections.
- Speaking of reflections, a high quality anti-reflective coating is especially helpful when prism is involved, as the thicker edge of the lens can create additional reflections, as do high-index lenses.
- As mentioned previously, whenever there is base-in prism, on either one or both lenses, it is important to ensure that the thick edge of the lens does not prevent nosepad adjustment.
APPARENT ALIGNMENT
Sometimes patients have no useful vision in an obviously deviated eye. There is no point in trying to “take the image to where the eye is” with prism, since the patient is functionally monocular. However, prism may still be able to help on an “appearance” basis. A prism oriented with the base toward the deviation (opposite direction of a prism designed to resolve diplopia) can render a more “aligned look.” For example, a base-out prism may make an exotropic eye appear to be straighter or turn out less. It is estimated that 8.0 diopters of prism will cause an apparent shift in the eye of about 1.0 mm. This can be useful, especially for those in the public eye. However, there are practical limits to this as the “base side” lens edge thickness increased quite a bit with the “8.0 diopter to 1 mm shift” estimate. This can perplex opticians as a patient may come in with an eyeglass Rx that calls for prism, in a direction that seems to be opposite from what would be expected (thinking that the prism is designed to correct diplopia).
CONCLUSION
There are many common and uncommon uses for prism in eyewear. Understanding the ways prism is prescribed will continue to be determined by the needs of patients, and the creativity and resourcefulness of the prescriber.



