KIDS, CONTACTS AND MYOPIA MANAGEMENT
A New Addition to a Comprehensive Myopia Management Protocol
By Linda Conlin, ABOC/NCLEC
Release Date: July 15, 2021
Expiration Date: July 14, 2024
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Describe the factors thought to contribute to myopia development and progression.
- Explain current methods of correction, including myopia management with contact lenses.
- Describe a new FDA approved 1 day contact lens for the early intervention and management of axial myopia.
Credit Statement:
NCLE 1 hour, Ophthalmic Level II, Course Number: CTWJHI107-2
 Myopia is more than a refractive error; it is more than shortsightedness; it is a progressive eye disease rapidly increasing globally, and there is no current cure. A recent article in Review of Myopia Management magazine points out that the cross-continental rapid increase of myopia fits the CDC definition of a pandemic. The immediate goal for ECPs is to correct the refractive error while managing and slowing myopia progression, beginning in early childhood.
Myopia is more than a refractive error; it is more than shortsightedness; it is a progressive eye disease rapidly increasing globally, and there is no current cure. A recent article in Review of Myopia Management magazine points out that the cross-continental rapid increase of myopia fits the CDC definition of a pandemic. The immediate goal for ECPs is to correct the refractive error while managing and slowing myopia progression, beginning in early childhood.
Left untreated in young children, myopia refractive error can affect normal early educational development, which has profound implications that can affect a child for life. Myopia management must also slow the progression to lower the risk of complications that pose a serious threat to eye health.
The exact cause(s) for the accelerated increase in myopia cases is still under investigation, but it is multifactorial. What is clear is the need to start comprehensive myopia management protocols in early childhood.
In this course, you will learn about the efficacy of contact lenses in managing myopia progression in children.
ALARMING STATISTICS
Between 1972 and 2004, myopia diagnosis increased by 66 percent. As a vision condition that affects more than 40 percent of the U.S. population, and more than 50 percent of the population in parts of Asia, it is the single most common vision condition in the world. If the current trend continues, the Brien Holden Institute predicts that nearly 50 percent of the world population, about 5 billion people, will be myopic by 2050. Myopia begins most often when children enter school and progresses through the teen years, with statistics indicating that the age of onset is decreasing.
EARLY INTERVENTION
According to American Optometric Association’s (AOA) evidence-based clinical pediatric guideline, parents should begin eyecare early, as early intervention is key to control its progression and combat the growing number of children struggling while living life out of focus every day.
Early intervention for normal Emmetropization (Normal Eye Development): Generally, myopia first occurs in schoolage children and progresses until about age 20. According to the AOA, 34 percent of children ages 12 to 17 are myopic. The Berkeley Infant Biometry Study (BIBS) documents the development of the major optical ocular components during emmetropization. The report examines how the major ocular components— namely axial length, corneal power and crystalline lens power—change to produce emmetropia and whether that process operates more by an active or passive process. Support for an active mechanism would come from evidence that emmetropization through modulation of axial growth is an active mechanism, whereas a passive mechanism would be emmetropization occurring primarily through modulation of corneal and lenticular power.
NEW TOOL MISIGHT 1 DAY
With FDA approval of a new soft contact lens MiSight 1 day, CooperVision provides the eyecare professional with a scientifically proven approach that complements a comprehensive myopia management protocol. MiSight 1 day addresses myopia progression by correcting axial myopia and its uncorrected contribution to the elongation of the eye. MiSight (omafilcon A) is a daily wear single use soft contact lens for the correction of myopic ametropia and for slowing the progression of myopia in children with non-diseased eyes, who at the initiation of treatment are 8 to 12 years of age and have a refraction of -0.75 to -4.00 diopters (spherical equivalent) with ≤ 0.75 diopters of astigmatism.
MYOPIA DEFINED
In normal eye growth referred to as emmetropization, the cornea and crystalline lens has the correct curvature and thickness to produce the correct refractive power to focus light on the retina of an eye of normal axial length without accommodation—any mismatch results in refractive error. If the focal length is too long, then hyperopia results; if the focal length is too short, then myopia results. In myopia, we know that light focuses in front of the retina resulting in blurred vision when viewing distant objects. There are two types of myopia: refractive and axial.
Refractive myopia occurs when one or more of the eye’s refractive structures produce a refractive error, such as when a steeper than normal corneal curvature or a thicker than normal crystalline lens exists and results in refractive power error where the power is too strong and produces a focal length that is too short for the eye’s focal length. This causes light to focus in front of the retina.
Axial myopia, however, is linked to the rapid increase in myopia progression and is the more common type of myopia. Axial myopia occurs when the length of the eyeball, or axial length, is greater than the focal length of the eye’s optical components.
The definition of myopia is a condition in which the spherical equivalent objective refractive error is more than –0.50 diopter (–0.50 D) in either eye, and high myopia is a condition in which the spherical equivalent objective refractive error is more than –5.00 D in either eye. Myopia has been connected to serious vision conditions such as premature cataract, glaucoma, retinal detachment and macular degeneration. As the degree of myopia increases, the risks increase exponentially for these eye health and sight-threatening complications.
High myopia is the most common cause of retinal detachment. Elongation of the eyeball due to axial myopia leads to areas of stretching and thinning that can eventually tear. Vitreous fluid seeps through the tear and causes the retina to detach from the choroid, the vascular layer of the eyeball between the retina and the sclera.
The elongation and stretching of the eyeball in high myopia can cause abnormal blood vessels to form in the macula, a condition called myopic choroidal neovascularization (MCNV). The leaking and scarring caused by CNV is a serious complication of pathological myopia as it is often a sudden onset with progressive decline in central vision. Recent studies have shown that even lower degrees of myopia, increase the lifelong risk of retinal detachment and macular problems.
FACTORS THAT MAY CONTRIBUTE TO MYOPIA PROGRESSION
As myopia management becomes more prevalent, it will be essential for ECPs to stay abreast of the current research and management protocols. To that end, we will address factors believed to influence the progression of myopia including environmental, diet, accommodative lag, genetics, disease, visually guided eye growth, hyperopic peripheral defocus and decoupling of the rate of growth of the crystalline lens versus eyeball growth.
ENVIRONMENT FACTORS THAT INFLUENCE AXIAL MYOPIA
The environment in which we use our eyes can play a part in myopia development. The amount of near work we do, time spent on computers, video games and texting, as well as less time spent outdoors all affect our eyes because the eyes accommodate to focus closer than in the relaxed state for distance vision. Research by the National Institute of Health (NIH) found that children spend about seven hours per day on entertainment media, including television, computers and video games.
More time in stationary activities leaves less time for outdoor activities, resulting in less exercise. Less exercise leads to higher blood insulin levels because the inactive muscles become resistant to insulin, which causes the body to produce more insulin. Increased insulin production results in amplified production of the hormone Insulin Growth Factor 1 – or IGF1. IGF1 causes increased scleral growth and possibly more eyeball growth.
Accommodative lag: Accommodation is the means by which the crystalline lens adjusts its shape to bring a near image into focus on the retina. When the accommodative response is less than the focusing demand, it is called accommodative lag. Accommodative lag can cause light to focus behind the retina, which may stimulate eyeball growth. Studies have investigated the effect that accommodative lag has on myopia progression in children, and there has been strong correlation between myopia progression and an increased accommodative lag. MiSight 1 day contact lenses with ActivControl Technology bring focus from behind the retina to the front.
VISUALLY GUIDED EYE GROWTH
Lack of exposure to natural light may play a part in myopia development, too. Exposure to sunlight may result in the production of dopamine, a chemical released by nerve cells to send signals to other nerve cells and inhibits eye growth. In addition, vitamin D, which we absorb from sunlight, may inhibit eye growth.
Visually guided eye growth is the process through which eye growth is naturally controlled to maintain normal vision. When light strikes the retina, amacrine cells—neurons that help regulate input from the photoreceptor cells—release chemicals that help slow scleral growth. In an experiment, chicks were raised in the dark and showed more eye growth than chicks raised normally.
Several recent human studies report that the time children spend engaged in outdoor activities is associated with a reduced risk of myopia. A 2019 study in Taiwan reported that children who engaged in outdoor activities for two hours per day or more exhibited a 50 percent reduced incidence of myopia, 32.9 percent slower myopic progression and 24.9 percent slower axial elongation. These findings and other studies suggest that children exposed to less than 60 minutes a day of bright outdoor light are at an increased risk of more rapid eye growth and myopia development, and that approximately two hours or more of outdoor exposure each day is required to provide protection against myopia development.
Exercise, time away from near tasks and exposure to natural light may all be factors in the results of an earlier study from Taiwan. For one academic year, a school required that all its students spend their recess time outdoors. Significantly fewer students in that school developed myopia than students of a nearby school who were not required to spend recess outdoors. Based on those results, both schools now require recess outdoors!
We know that daylight hours vary by latitude. In higher latitude countries such as Denmark, daylight hours are short in winter, but very long in summer. This presented an opportunity to study eyeball growth, or axial growth, based on hours of sunlight by season. During the winter, axial growth was 0.07 mm more than during the summer.
NEAR VISUAL DEMAND
Near work for prolonged periods may cause images to focus behind the retina and stimulate eye growth. A German study examined the connection between myopia and level of education—presumably, the level of education indicated the amount of close work required. Researchers examined more than 4,000 adults. They found that the incidence of myopia increased with the level of education, with 53 percent of university graduates myopic as compared with only 24 percent of those who had no secondary education. The recent World Health Organization (WHO) guidelines recommend a maximum of three hours per day spent on close work and screen time, increased outdoor and physical activity and implementing the 20/20/20 rule: After 20 minutes of near or screen work, gaze at something 20 feet away for 20 seconds.
GENETICS
Genetic factors contributing to myopia are being studied. In addition to other genes and chromosomes under consideration, the PAX6 gene may have a connection with the body’s production of a chemical that controls eye growth. Other evidence indicating a genetic factor is that East Asian countries have the highest incidence of myopia—96 percent of Korean 19 year olds are myopic—and African Americans the lowest.
Most infants are born with low to moderate hyperopia. With genetic predisposition, children can be mild to moderately myopic at age 5, while myopia has not appeared in children of the same age with no genetic predisposition. At school age, reading and close work begin and can trigger myopia in both groups. Between ages 8 and 14, children in both groups are myopic, but those with no genetic predisposition have mild to moderate myopia, while those with genetic predisposition are moderate to high myopes. Continuing to college, postgraduate studies and occupations requiring close work at ages 20 to 25, the group with genetic predisposition are now high myopes, while the group without genetic predisposition remained mild to moderate myopes.
LEPREL 1 is another gene associated with myopia. LEPREL 1 encodes an enzyme that modifies collagen in the eye. A mutation in that gene results in the absence of the enzyme. An excess of collagen develops, and the eye elongates. Collagen is a protein found in fibrous tissue like the sclera. When there’s too much collagen, the sclera grows, and the eyeball elongates.
Advances in gene sequencing and access to large biobanks are likely to yield more information about genetic predisposition to myopia.
DISEASE
A small number of patients under age 20 are diagnosed with glaucoma each year. The elevated intraocular pressure (IOP) associated with glaucoma causes the eyeball to stretch, resulting in myopia. With congenital glaucoma, when the IOP returns to normal, normal eyeball growth returns, too.
Glaucoma is also associated with Stickler Syndrome, a genetic condition. The syndrome is the result of the mutation of several genes affecting collagen production, which in turn affects the eye shape, resulting in myopia.
PERIPHERAL HYPEROPIC DEFOCUS
Here’s a term that’s fun to say: peripheral hyperopic defocus. Dr. Earl Smith, the Dean of the University of Houston College of Optometry, conducted groundbreaking research that changed our understanding of myopia progression. His research shows that peripheral hyperopic defocus stimulates eye growth, while peripheral myopic defocus was the stimulus to slow eye growth.
Fig. 1 shows an illustration of peripheral defocus.
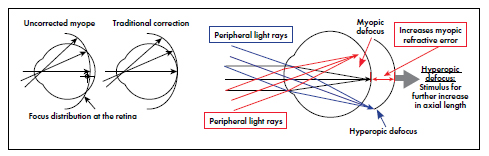
FIG. 1
DECOUPLING
Decoupling may be another factor in myopia. It is a mismatch in the growth of the optical elements of the eye with respect to the eye’s axial length. In children with normal vision, the crystalline lens thins and flattens with growth. In children who develop myopia, a study at the Ohio State College of Optometry found that the lens stopped changing about a year before myopia onset. More research is needed, but decoupling is a possible cause of defocus, as is an abnormal eyeball shape and an abnormally thick ciliary muscle. Abnormal eye shape or ciliary muscle thickness can form a mechanical restriction preventing the stretching that thins and flattens the lens as the eye continues to grow.
NO CURE, BUT CONTROL
What can be done to control myopia? Rigid gas permeable lenses flatten the cornea, shortening the axial length. But when the lenses are no longer worn, the cornea resumes its original shape. A National Eye Institute Contact Lens and Myopia Progression study (CLAMP) found that flattening the cornea doesn’t prevent the root cause of myopia, which is eyeball growth.
ORTHOKERATOLOGY
Orthokeratology, or ortho-k, is currently considered an effective strategy for myopia control. It is the fitting of specially designed gas permeable contact lenses that are worn overnight to reshape the cornea. Orthokeratology lenses have a much flatter central base curve than the secondary curve, redistributing the corneal epithelial cells peripherally while flattening the central cornea. Through this plateau-shaped cornea, light is refracted simultaneously onto the midperipheral retina and macula, leaving the peripheral retina with relative myopic defocus in front of the retina. Moving peripheral defocus from hyperopic to myopic is believed to stabilize eye growth and reduce myopia progression.
An appealing benefit to orthokeratology is that the lenses are worn only overnight, so glasses or contact lenses aren’t needed during the day. However, studies have shown that discontinuing overnight lens wear before at least two years of therapy results in resuming myopia progression and axial growth. What’s more, G.P. lenses require care, so parental supervision is necessary for younger patients.
Like ortho-k, CooperVision Paragon CRT (Paragon Vision Sciences) is a specific brand of corneal reshaping lenses that have a proprietary lens design and fitting methodology, called corneal refractive therapy (CRT). Though technically different from orthokeratology, CRT is used for similar purposes and produces comparable results.
Central corneal flattening with CRT results in a thicker area at the peripheral cornea. Because of that increased thickness, peripheral focus is brought from behind the retina to the front of it, called peripheral myopic defocus. As in orthok, changing the peripheral focus from hyperopic to myopic is thought to slow myopic progression.
ACCOMMODATIVE DEMAND
Accommodative demand is the dioptric power needed to focus on an object at a particular distance. The closer the object, the greater the accommodative demand. It has long been thought that by relieving some accommodative demand, bifocal lenses would help slow myopia progression. Bifocal spectacles, while they slow myopia progression a small amount, are not as effective in myopia control as other strategies.
Multifocal spectacle lenses also have been shown to slow myopia progression somewhat, but it isn’t certain whether the relief of accommodative demand at a greater variety of distances, or correction of peripheral defocus is responsible. Studies of vision training in conjunction with multifocal lenses have shown promising results.
Multifocal contact lenses used off label, however, have shown more success. Studies using concentric lens designs with distance center showed a 50 percent or better reduction in myopia progression and 29 percent or better reduction in axial growth. The concentric design yields simultaneous distance and defocus correction. Progressive designs with central distance correction and a plus periphery to induce myopic defocus did not perform as well in studies as the concentric designs. The Vision Cooperative Research Centre in Australia designed a way to independently focus central and peripheral images with a multifocal contact lens with a peripheral add.
Now we have CooperVision’s MiSight 1 day soft contact lens, which won FDA approval in November 2019. It is the first FDA-approved product clinically proven to slow the progression of myopia when initially prescribed for children 8 to 12 years old. In a three-year clinical trial, this daily disposable lens reduced myopia progression by 59 percent when compared to single vision contact lenses, in addition to a 52 percent reduction in axial lengthening.
MiSight 1 day slows elongation of the eye through ActivControl Technology. This concentric design has two corrective zones to correct myopia in all gaze positions and two treatment zones to change hyperopic defocus to myopic defocus to slow axial elongation. CooperVision added the Brilliant Futures Myopia Management Program to make MiSight 1 day a comprehensive myopia management program. Brilliant Futures is an education and support tool for parents and children when this lens is prescribed. The program employs a mobile app to keep patients engaged with their eyecare practitioner and the program to create a new standard of care for children with myopia. It provides inclusive practice, child and parent support to create the optimal environment for compliance, satisfaction, clinical outcomes and long-term loyalty, all via a comprehensive management program featuring MiSight 1 day daily disposable contact lenses.
At this time, CooperVision has conducted the longest-running clinical trial of pediatric contact lens wear, more than six years, with MiSight 1 day. More than 80 percent of children in the trial reported insertion and removal of the lenses as “easy” and preferred wearing contact lenses over spectacles for daily activities. As a daily disposable lens, there is no training needed for care and cleaning, adding convenience to the vision benefits. Early myopia management is key with kids and teens. The Adolescent and Child Health Initiative to Encourage Vision Empowerment (ACHIEVE) study revealed that contact lenses can greatly enhance a young person’s self-esteem.
EARLY INTERVENTION
As with many other physical conditions, early intervention has been found to be key in slowing myopia progression. The AOA recommends myopia correction and control measures begin early in life. Early-onset myopia is linked to more rapid progression and development of high myopia. High myopia increases the risk of retinal detachment, cataracts, glaucoma and other conditions. It is critical to identify candidates for myopia progression and put preventative measures and treatments in place early.
The Myopia Institute White Papers compiled research showing that the risk of high myopia is most significant with early-onset. It is the current best determinant for identifying children at risk for progression.
The Brien Holden Institute in Australia has done extensive research on the causes of myopia and its control. They developed a Myopia Calculator, in which you enter the patient’s age and refractive error to predict the patient’s refractive error by age with and without management with multifocal contact lenses.
CONCLUSION
Research continues into the causes of myopia, and as the causes become clear, pathways to treatment and prevention open. Current areas of study are genetics, pharmaceuticals, combination treatments, treatment schedule and individualized treatment plans that consider many factors, such as the age of onset and degree of myopia. Early action is key to slowing myopia progression, since the earlier the onset of myopia, the more rapid its progression to high myopia. Action includes educating parents about myopia: what it is, why it happens and the long-term eye health complications and risks.

