Controlling Myopia in Children
By Barry Santini, ABOM
Release Date: May 15, 2015
Expiration Date: February 10, 2020
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Understand the growing incidence of myopia and results of current research.
- Learn why controlling myopia in children is important for an optician to know.
- Know the acceptable ways used to control the progression of myopia.
Faculty/Editorial Board:
 Barry Santini, A.A.S., ABOM, is a New York State licensed optician, is ABO certified and was awarded an ABO Master in 1994. He has been an owner of Long Island Opticians in Seaford, N.Y., from 1996 to present.
Barry Santini, A.A.S., ABOM, is a New York State licensed optician, is ABO certified and was awarded an ABO Master in 1994. He has been an owner of Long Island Opticians in Seaford, N.Y., from 1996 to present.
Credit Statement:
This course is approved for one (1) hour of CE credit by the American Board of Opticianry (ABO). Course STWJH602-2
Within the last 20 years, both the prevalence of myopia and its rate of increase within the world’s population are rising. It is estimated that 33 percent of the U.S. population is myopic—defined as greater than -0.50D and can range up to 80 percent in some Asian countries like Singapore and Taiwan. Particularly in the case of school-aged children ages 7 to 17, many industrialized areas of the world are experiencing rates of increase in myopia approaching 50 percent... a number that cannot be simply explained by genetic or environmental factors alone.
As a group, young people with myopia are at risk. The negative cognitive, neurological, social, behavioral and economic effects that often accompany uncorrected myopia can have long-term, life-altering impact, especially if their visual impairment remains latent or goes untreated. This is compounded by these two facts: Children often have little awareness of their own vision deficiencies, and they also lack the ability to clearly articulate the exact nature of their vision problems.
WHY CONTROL MYOPIA IN CHILDREN?
Controlling myopia in children is important. According to the World Health Organization, whose global health initiative currently places particular emphasis on correcting refractive conditions early, children with myopia progressing beyond 5 diopters can become adults who are more predisposed to developing glaucoma, cataracts, macula degeneration, retinal holes and tears, as well as detachments of vitreous and retina. And while farsightedness is almost always present at birth, infantile hyperopia decreases in magnitude for most by age 4, while by age 15, almost 15 percent of children have developed some degree of myopia.
According to noted myopia researcher Jeffrey Cooper, OD, the prevalence of myopia in young American adults has increased from 25 percent in 1971 to 1972 to over 41 percent in the period between 1999 to 2004. In Taiwan, the incidence of myopia affects between 60 percent and 80 percent of young adults and around the world averages 50 percent or more in adolescents—providing strong evidence that something more fundamental than local environmental factors or simple genetics are at work in influencing myopic progression.
BIG CONSEQUENCES
The long-term consequences of neglecting our children’s visual health are manifold and significant. In a 2008 study titled “A Call to Action” underwritten by the Essilor Vision Foundation, Dr. Joel N. Zaba describes the consequences of being complacent about a child’s vision error:
“Children with undiagnosed and untreated vision problems grow up to become adults with undiagnosed and untreated vision problems. The failure to detect and treat vision disorders in children affects, among other things, such issues as childhood development, learning performance, self-esteem, social-emotional behavior, academic achievement, high school drop-out rates and juvenile delinquency. From the standpoint of society in general, the failure to detect and treat children’s vision disorders affects the rates of adult criminality, literacy and labor productivity.”
POOR GATEKEEPING
Along with the discovery that myopia is rapidly increasing in our young population, we are beginning to recognize how insubstantial our gatekeeping has been in safeguarding our children’s eye health. Although we know that 80 percent of what a child learns comes through their eyes, our society has been slow to institute the changes necessary for improving our children’s visual performance. To illustrate this, here are 10 quick facts regarding myopia and the general eye health of our children:
- Only 7 percent of children receive a complete eye exam by the first grade.
- Up to 66 percent of all children receive no type of preventive vision care, including simple screenings, before they enter the first grade.
- Only 50 percent have had a complete eye exam by the time they graduate high school.
- Twenty-five percent of children have a vision problem that interferes with their ability to learn.
- School screenings are only effective in identifying 5 percent of vision problems. 6. Up to 67 percent of children who fail a school screening do not receive a follow-up exam by an eye doctor.
- Annually, about 7.5 million children who are visually impaired go untreated.
- The mean annual myopic progression is between 0.50D - 1.00D.
- Myopic onset begins around age 6 and dramatically slows around age 16.
- A 0.25D annual rate of myopic progression is considered clinically relevant.
In the United States, the National Parent Teacher Organization estimates that more than 10 million children suffer from vision problems that can result in poor academic performance.
THE EYE AND MYOPIAWhen parents arrive with their teenager in tow for a scheduled eye checkup, an oft repeated question is revealed: "We came in for our yearly checkup, and we just knew we'd be getting a new Rx again. Doctor, can you tell me why their eyes are getting worse every year?" In order to provide the best answer, a working knowledge of the eye and its development during the first 10 years of life is essential. All babies are optically farsighted at birth. Although the newborn's eye has an axial length and globe size averaging 8 mm and 75 percent less than an adult eye, it is compensated by:
But what happens to them as their bodies experience the rapid physiological growth normal in the first 10 years of life? How does nature react to coordinate the various optical elements within the eye to help keep an image in focus? EMMETROPIZATION THREE NATURAL PROCESSES
KEEP FOCUS IN CHECK THE POWER OF THE PERIPHERAL RETINA Foveola—A 0.35-mm diameter area centered within the fovea centralis of the retina, featuring the greatest density of cones and containing no rods. Its area subtends a 1-degree field of view (FOV). The foveola is capable of seeing the highest degree of visual acuity (20/08), based on its retinal mosaic density.
Macula—A 6-mm diameter area roughly centered in the retina and temporally placed to the optic nerve. It represents just 5 percent of the total area of the retina and subtends a 15 to 18-degree FOV. It features a mix of rods and cones.
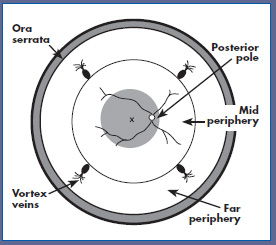
POLAR MAP PROJECTION OF THE EYE |
But now, with the advent of the Affordable Care Act, we have taken the first steps to address the deficits in our vision gatekeeping. Under the ACA, eligible children are now fully covered for yearly eye health exams up to the age of 19. Because eyecare professionals will now begin to see far more children passing through their doors far more frequently, they’ll need to make boning up on the latest theories, research and treatments concerning arresting myopic progression an essential part of their continuing education.
WHAT’S CAUSING THE INCREASE IN MYOPIA?
Here the experts rarely all agree, Most feel that parental genetics are important in determining whether any individual becomes myopic, but in view of the worldwide increase in myopia, researchers often place genetics behind these common suspects:
- An increase in the amount of time children spend on close-focus activities.
- An increase in the amount of time spent using mobile devices.
- A decrease in the amount of outdoor activities under bright sunlight.
- The newly-recognized importance that peripheral retinal blur can initiate processes resulting in increased axial growth.
Let’s look at these factors one by one:
- Increase in close-focus activities: Although not universally agreed upon, many myopia experts feel that the increased accommodative tension encountered during sustained close focus tasks weakens aspects of the scleral attachment to the ciliary body, thereby allowing it to stretch or elongate.
- Increased use of mobile devices: These devices, which are typically held 3 to 4 inches closer to the eye than the normal distance of 16 inches, place additional accommodative and convergent demands on the eye. It is also thought that the light emissive nature of mobile device screens may produce a negative compounding effect on the peripheral retinal images during close tasks and perhaps stimulate axial growth.
- Decreased outdoor activities: Here theories infer that exposure to sunlight narrows the pupil and therefore reduces peripheral blur through the pinhole effect. Other studies suggest that some wavelengths of sunlight have a beneficial effect by increasing retinal dopamine production, which is thought to help meditate axial growth. There appears to be a correlation between the weekly hours children spend in sunlight activities and the degree of myopic progression.
- Peripheral hyperopic induced blur: The peripheral image shell formed in the eye of a well-corrected or under-corrected myope through the use of best form lenses is hyper-opic in nature and therefore found behind the retina. As the peripheral retina’s photosensitive and processing cells have evolved to seek images with the best edge gradients and highest contrast, mechanisms in the eye have been created that automatically try to extend the peripheral retina rearward in order to obtain optimal contrast in the image plane. The end result is an axial elongation of the rear scleral shell, resulting in increase in myopia.
CONTROLLING THE MYOPIC PROGRESSION
When measuring the efficacy of myopia-controlling treatments, today’s researchers are using a metric based on quantifying and comparing changes in the axial length of the eye or more specifically, the change in the depth of the vitreous chamber. Amongst the most important current tenants in research surrounding myopia control is that one cannot completely stop the myopic progression. Below is an overview of the primary treatment avenues that researchers have investigated in their efforts to slow or arrest the rate of myopic progression:
- Relieving accommodative effort: Historically, both bifocal and progressive spectacle lenses have been employed to reduce the myopic progression by targeting a reduction in accommodative effort, albeit with mixed results. Parents have often intuited that under correcting the myopic error in spectacles would reduce its progression, but studies have shown that not only is this largely ineffective, it has, in many cases, actually increased the total myopia observed. Alternately, bifocal contact lenses have been shown to offer statically significant reductions in the rate of myopic progression in many studies (see Ortho K below).
- Reducing the neuro-retinal triggers stimulating axial growth: With respect to reducing
peripheral hyperopic blur as a key trigger, spectacle lenses have been developed that employ
an alternate peripheral aberration correction
and have been shown to be a statistically-significant treatment in reducing myopic progression, Carl Zeiss distributes a version of this lens,
called MyoVision, in various markets around
the world, but not currently the United States.
Additionally, progressive and bifocal contact
lenses have been specifically used to target
reducing peripheral hyperopic blur and have
delivered clinically significant results.
- Corneal reshaping: Known variously as Orthokerantology (OK), Ortho-K, Corneal Reshaping Treatment (CRT) and Vision Shaping Treatment (VST), this modality uses a rigid, reverse-geometry design, oxygen-permeable contact lens that is worn overnight. It is designed to flatten the central cornea while steepening the periphery, thereby simultaneously attempting to deliver an improved foveal focus while reducing peripheral hyperopic blur. Overall, studies have shown up to a 40 percent reduction in axial length gain through corneal reshaping treatment.
- Anti-Muscarinic Therapy: Atropine and pirenzepine are also thought to mitigate the action of the neural-retinal growth trigger in the scleral shell. These drugs, however, even in low dosages sometimes produce unwanted side effects in selected individuals. Their long-term efficacy for use with children is unknown.
THE EVIDENCE IS CLEAR
In view of the documented negative health, behavioral and economic impact portended by the worldwide increase in the incidence of myopia, it is essential that all eyecare professionals and staff, from eye doctors to healthcare technicians to even dispensary personnel, keep up with the latest information on controlling myopic progression in children. The following studies stand out and merit your attention: the Correction of Myopia Evaluation Trail (COMET); Children's Overnight Orthokera-tology Investigation (COOKI); The Contact Lens and Myopia Progression study (CLAMP); the Corneal Reshaping and Yearly Observation of Nearsightedness study (CRAYON); the Longitudinal Orthokeratology Research in Children study (LORIC) and the forthcoming Stabilization of Myopia by Accelerated Reshaping Technique trial (SMART).
Understanding and early intervention is the key toward addressing the world’s growing myopia epidemic. The journey to realizing the joys and rewards of helping reduce the negative impact of myopia are easy for both parents and professional, and begins at www.myopiaprevention.org.
Special thanks to Dr. Saulius Varnas and Dr. Stephen Silberberg for their help and time taken to provide their expertise on the science of myopia control.


 Fovea Centralis—A 1 to 1.5-mm diameter area centered within the macula, representing only 1 percent of the total area of the retina. Its area subtends a 3 to 5-degree FOV. The fovea is literally a numerical Game of Fives:
Fovea Centralis—A 1 to 1.5-mm diameter area centered within the macula, representing only 1 percent of the total area of the retina. Its area subtends a 3 to 5-degree FOV. The fovea is literally a numerical Game of Fives: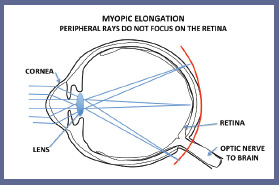 Peripheral Retina—Defined as all the retinal real estate outside the macula, it is separated into the mid-peripheral and far peripheral areas by its equator. The equator is defined as a circle subtending the largest dimension of the globe and whose origin is located on the anterior-posterior pole. It represents approximately 67 percent of the globe's inner surface, making it by far the largest area of the retina. Starting approximately 18 degrees from the fovea, the peripheral retina extends to the ora serrata, the junction between the retina and the ciliary body. The visual acuity of the peripheral retina decreases rapidly as we move away from the macula and is overall, many, many times worse than the fovea. The limits of peripheral retina define an FOV of 100 degrees vertical and 120 degrees horizontal. Comprised of mostly rod photoreceptors, there are additionally present 1 to 3 percent of ganglion cells that also have photoreceptive properties. The ganglion cells found in the mid peripheral retina layers are thought to be responsible for autonomic management of circadian rhythms and pupillary reflexes.
Peripheral Retina—Defined as all the retinal real estate outside the macula, it is separated into the mid-peripheral and far peripheral areas by its equator. The equator is defined as a circle subtending the largest dimension of the globe and whose origin is located on the anterior-posterior pole. It represents approximately 67 percent of the globe's inner surface, making it by far the largest area of the retina. Starting approximately 18 degrees from the fovea, the peripheral retina extends to the ora serrata, the junction between the retina and the ciliary body. The visual acuity of the peripheral retina decreases rapidly as we move away from the macula and is overall, many, many times worse than the fovea. The limits of peripheral retina define an FOV of 100 degrees vertical and 120 degrees horizontal. Comprised of mostly rod photoreceptors, there are additionally present 1 to 3 percent of ganglion cells that also have photoreceptive properties. The ganglion cells found in the mid peripheral retina layers are thought to be responsible for autonomic management of circadian rhythms and pupillary reflexes.
