 By Linda Hardy, LDO- GA, CPOT, COA
By Linda Hardy, LDO- GA, CPOT, COAIt’s not every day that you see a patient with a choroidal melanoma. Even though I have been in this field for over 20 years, I have seen only two cases. Each time it is alarming and scary to know what the patient will be enduring, the longevity of treatments and continual care with a retinal specialist, and the possibility of enucleation. The most recent case of choroidal melanoma in which I assisted has left me feeling more positive about the future care for these patients.
In February 2017, a 55-year-old Caucasian male was in the office for a routine eye exam and fitting for gas permeable contact lenses. During his case history, the patient explained that he had noticed flashes of light and increased floaters in the right eye for approximately six months. His biggest concern was a large floater that didn’t move like the others; it remained in one place and was constant.
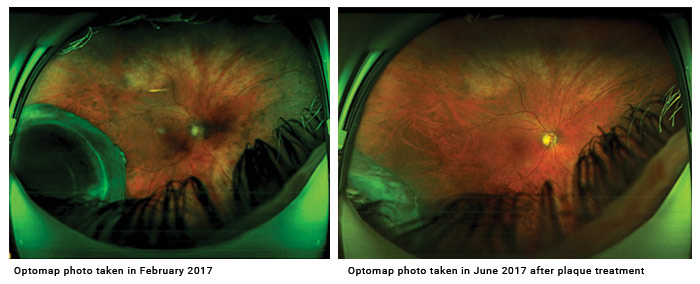
The patient’s corrected visual acuity was 20/40. We performed Optomap Retinal Imaging on both eyes. What we found was shocking, especially when this patient was seen less than a year earlier for a complete exam including Optomap photos and dilation, with no complications.
Of course, the patient was immediately referred to a retinal specialist. A B-scan was performed and the echo graphic finding was consistent with a choroidal mass. The patient returned to see another retinal specialist for a second opinion. The B-scan was repeated along with the dilated evaluation. It confirmed that the patient had a choroidal melanoma. The tumor was 8.32 mm in length and 16.4 mm in width.
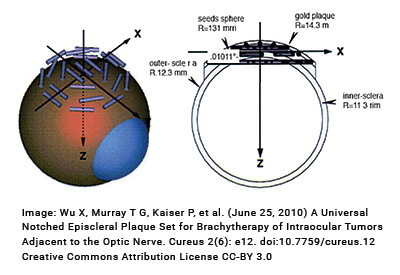
The retinal specialist had a long discussion with the patient regarding the tumor. Although the tumor was sizeable, it was treatable with plaque therapy. This treatment delivers a highly concentrated radiation dose to the tumor, with less radiation to the surrounding tissues. The radioactive plaque is also called a radiation implant.
The radiation is in the form of a rice-sized radioactive seed. The seeds are attached within a gold or steel bowl called a plaque. The dose of radiation delivered depends on the size of the tumor and its location. Placement of the plaque is performed in the operating room. The surgeon attaches the plaque to the wall of the eye covering the base of the intraocular tumor.
After the surgery, the retinal doctors followed the patient closely. After two months, he was healing well, and the doctors saw early regression of the tumor. The tumor is a class 2 tumor with higher likelihood of metastasis.
By June 2017, the tumor had shrunk in size to 4.42 mm in length and 10.84 mm in width. The tumor is inoperable, but treatable. The man will be evaluated every few months for the rest of his life to make sure the tumor does not grow. But he will live with both eyes, his vision correctable to 20/20 in the right eye currently. He will also know that the tumor is not spreading to other areas of his body including his brain. These advancements in technology are amazing and give hope for future advancements.













