
By Jeff Hopkins
While progressive lenses are an eternal topic in our industry, single vision lenses are often overlooked. It’s easy to see why: The product category is literally ancient, and the great majority of single vision lenses sold can be considered a commodity product. However, the latest single vision lenses and other new types of lenses for younger wearers are as advanced in technology as the latest progressive lenses. And the innovations they embody could benefit many younger eyeglass wearers—if only they knew about them.
ORIGINS
Single vision lenses were, of course, the original spectacle lenses. Exactly when they were invented is not known for certain; the first reference we have to spectacles is, oddly enough, in a sermon delivered in 1306 by Friar Giordano de Pisa. He wrote, “It is not yet 20 years since there was found the art of making eyeglasses, which make for good vision.” (This could also be the first example of a celebrity eyewear endorsement.) These early eyeglasses had convex lenses that could provide reading vision for presbyopes and correct hyperopia (Fig. 1). Concave “minus” lenses for myopia began to appear in the 16th century, and the first lenses with cylinder power for correcting astigmatism were developed in the early 19th century. Obviously, the early evolution of lenses moved slowly.
ASPHERIC AND ATORIC SINGLE VISION
It was much later that lenses evolved beyond strictly spherical curves, but the need was there. Spherical lenses provided excellent vision if the most appropriate base curve was used for the patient’s prescription. However, for stronger prescriptions, a spherical lens could be thick and bulgy. One way to address this was to use a lens with a flatter front curve. However, since this would not be the ideal front curve for the prescription, the wearer would not have clear vision across the full height and width of the lens (how much it was restricted depended on the patient’s prescription and the curve chosen.) In short, wearers with stronger prescriptions had to choose between the need to see well and the desire to look good.
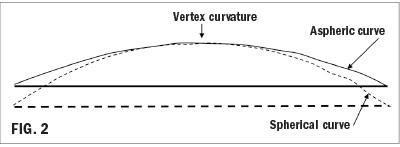
In the 1950s, a solution was developed that greatly reduced the need for compromise: aspheric lenses. This type of lens has a curvature that “flattens out” between the center of the lens and the edge (Fig. 2). The changing curvature creates surface astigmatism that counteracts the peripheral astigmatism that the wearer would encounter away from the center of the lens with a typical flattened curve. Wearers could enjoy lenses with a thinner edge (minus lenses) or a thinner center (plus lenses), without the other unfortunate aesthetic effect of strong spherical lenses: making the eyes appear abnormally large for hyperopes or small for myopes. Today, aspheric single vision lenses coexist with spherical lenses, providing an appealing alternative for wearers with stronger prescriptions.
However, even aspheric lenses had a shortcoming: They could not be optimized for both sphere and cylinder power. That means that patients with astigmatism (once again, especially in higher powers), would not have clear vision throughout the entire lens. And since about 70 percent of all eyeglass wearers have astigmatism, a lot of people weren’t seeing their best.
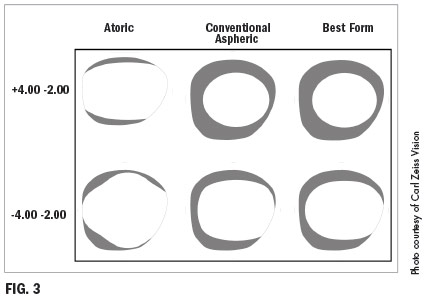
A technologically advanced, but not widelyused solution came in the form of atoric lenses. An atoric lens is aspheric in both the spherical and cylindrical meridians of the lens. That meant, essentially, that they could be optimized for wearers needing both a spherical correction and an astigmatic correction (Fig. 3). Unfortunately, this “asphericity squared” meant that the lenses could not be surfaced with the lab tools available at the time. The lenses usually had to be manufactured in “finished” form, and as a result, they had limited availability and were expensive.
With traditional manufacturing and surfacing technologies, aspheric and atoric designs were about as far as single vision lenses could go in terms of innovation. Atoric lenses were a high-value category, but the combination of limited availability and a relatively high price meant that they never took off in the market. Spherical and aspheric lenses have become a commodity product with little performance distinction among different brands. As a result, the main competitive differentiation has become price; today these lenses are low cost and offer relatively low profits for eyecare practices compared to progressive lenses. With virtually no technological breakthroughs to talk about, they more or less became an invisible product.
ENTER FREEFORM MANUFACTURING
The advent of freeform manufacturing for eyeglass lenses opened up new possibilities, revolutionizing single vision lenses just as it has done for progressive lenses.
To understand the difference that freeform manufacturing has made, we need to briefly look at the traditional approach to manufacturing lenses. Traditional single vision lenses are manufactured in one of two ways: Finished, meaning that the lens design and the prescription power were molded into the lens by the manufacturer; and semi-finished, where the lens design (front surface) was molded by the manufacturer, and the prescription was applied to the back surface by the lab, using symmetrical spherical and cylindrical tools. These manufacturing approaches still account for the great majority of single vision lenses.
Freeform manufacturing is a far more flexible manufacturing process. In freeform, a computer-driven, single-point diamond cutting tool is used to apply both the design and the prescription to a spinning plastic “puck” with a front curve only. A freeform generator can apply virtually any curve, no matter how complex, to a puck, allowing it to be free of the restrictions of traditional surfacing.
FREEFORM CUSTOMIZATION
Freeform shifts the main part of the manufacturing effort from the factory to the freeform-enabled lab, where the lens can essentially be created in real-time, after the lens has been ordered. Therein lies the key to the benefits of freeform: If the lens can be manufactured after the ECP has placed the order (effectively in real-time), the design can also be modified based on information specific to the individual patient. That means that a unique customized lens can be designed and manufactured for the needs of each wearer.
Why does that matter? It’s easy to assume that because there has been so little evolution, traditional single vision lenses must offer the best visual experience possible. However, single vision lenses have suffered from inconsistent performance and visual limitations that are in some ways similar to those experienced with traditional progressives.
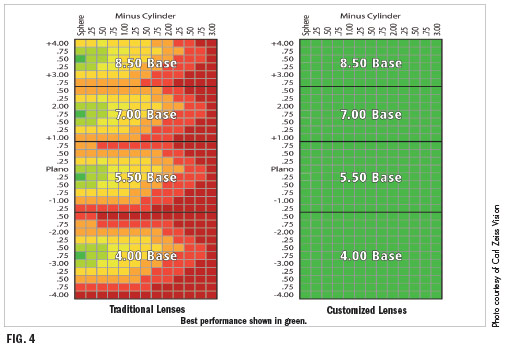
One limitation comes from the use of standard base curves. Readers familiar with Tscherning’s Ellipse will recall that there is an ideal base curve for every sphere power. However, the limitations of the traditional manufacturing, distribution and inventory process meant that only a few base curves had to cover the entire range of sphere powers. Patients with prescriptions that corresponded closely to a base curve would enjoy the best vision, but for those whose prescriptions are near the edge of a base curve range, the areas of clear vision were limited. The limitations were more acute for patients with stronger prescriptions.
Freeform lenses, also known as digital lenses, still use lens pucks with a limited number of base curves. The difference is that through real-time customization, compensation can be added to the design that “bridges the gap” between the ideal base curve for the prescription and the actual curve on the lens puck. The effect is as if every patient were receiving a lens made with the ideal base curve for the prescription. This will result in larger fields of clear vision for many wearers and consistently excellent performance across the full prescription range (Fig. 4).
The problem is even more significant for patients with significant amounts of astigmatism. As mentioned before, optimizing for both sphere and cylinder powers requires an atoric lens; these lenses are difficult to manufacture and have limited availability. With freeform manufacturing, however, lenses can be made atoric as part of the surfacing process, greatly improving the visual experience for patients who have astigmatism.
Another advantage of freeform is the ability to account for the position in which the lenses are worn by the patient. This wearing position is a result of the interaction between the frame chosen by the patient and the patient’s facial features. The distance between the front of the eye and the back of the lens (vertex distance), the vertical tilt of the frame (pantoscopic angle) and the horizontal curve of the frame (face-form wrap) can create a difference between the powers prescribed by the doctor and the powers experienced by the wearer.
The freeform customization process allows the wearing position to be considered in the design of the lens, resulting in lens powers that are compensated for the position of wear. As a result the powers of the lens are not the exact powers prescribed, but allow the patient to experience the effect of the prescribed powers when wearing the lenses. This means sharper vision for the patient than can be provided with uncompensated lenses.
This type of compensation has two implications for the dispensing of eyewear. First, the dispenser must measure the vertex distance, pantoscopic angle and frame wrap with the patient wearing the chosen frames. This can be done with manual tools, but is ideally performed with a digital centration device, such as the ABS Smart Mirror or Zeiss’ i.Terminal 2.
Lenses delivered from the lab will include a sheet showing the prescribed powers along with the compensated powers. This requires the dispenser to trust that the powers were compensated correctly, but ultimately it is the only way for the patient to receive the precise visual experience that the doctor intended.
BEYOND SINGLE VISION: AUGMENTATION FOR YOUNGER WEARERS
The development of the original single vision lenses was in part an acknowledgement of one of the difficulties of civilized living: reading is challenging to the eyes, especially older eyes. In contemporary life, the challenge is even greater, thanks to the almost universal use of digital devices among Americans of all ages. These challenges don’t just affect those who have reached the traditional age of presbyopia; they affect younger wearers as well. In fact, the greatest number of complaints about digital eyestrain come from wearers under 40.
One problem is that digital screens don’t have the clarity or contrast of printed pages, and pixels that comprise a digital image (either of text or graphics) can be confusing to the eye. In addition, on average we check our smartphones about 52 times per day, and the constant refocusing required can tire the eye’s ciliary muscles, causing fatigue.
Another issue relates to how we hold a smartphone or other handheld device. On average, we hold the phone about 25 percent closer to the eye than we tend to hold printed matter. We think of presbyopia as beginning when we can no longer hold reading material far enough away to see it clearly. But the decline in near visual acuity actually begins when we are quite young, and the nearest point on which we can focus continually moves farther away. Since we hold smartphones closer than books, it only makes sense that we lose the ability to focus comfortably on them earlier in life. That means that people below the traditional age of presbyopia who are heavy smartphone users can experience presbyopia-like symptoms that a conventional single vision lens can’t relieve.
The solution is a lens that provides distance vision with an area of low add, typically 0.50 to 1.00 diopters, below the 180 line. This digital “bump,” positioned for the typical viewing angle of a handheld device, alleviates some of the eye’s focusing effort, relieving symptoms of digital eyestrain (Fig. 5). These lenses are sometimes called relaxed vision lenses, enhanced single vision lenses or anti-fatigue lenses. Technically, they are progressive addition lenses because the power changes as the eye moves downward. But the low adds used limit peripheral astigmatism, which, combined with the careful positioning of the area of add power, allow the lenses to maintain the single vision feel that younger wearers demand. Studies have shown that this type of lens can significantly reduce digital eyestrain among wearers.

SELLING ADVANCED LENSES TO PRE-PRESBYOPES
Clearly, customized single vision and augmented single vision lenses offer significant advantages to many wearers. And yet, sales of both categories remain relatively low. According to the Premium Lens MarketPulse survey (see the May 20/20 issue), only 24 percent of ECPs said that digitally enhanced single vision lenses comprised more than 15 percent of their single vision lens sales, while 27 percent said the number was less than 3 percent. Digitally enhanced progressives, on the other hand, averaged 48 percent of progressive lens sales. (The survey did not include data for relaxed vision lenses.)
The question is, “Why aren’t more of these lenses being sold?” The most likely reason is that few single vision wearers are aware of them. That’s really not a patient problem, since they rely on eyecare professionals to keep them abreast of new beneficial lens technologies. But dispensers may not be talking about them—likely because they don’t think single vision wearers will pay significantly more (perhaps twice as much) for their eyewear compared to standard single vision lenses. Below are some tips that might help increase sales of these advanced lenses.
Don’t make assumptions. A common piece of advice in the lens business is “stay out of the patient’s wallet.” In other words, don’t make assumptions about how much the patient is willing to spend. Some younger patients may not be able to afford more expensive lenses, but there are plenty of single vision wearers in their late 20s and 30s with disposable incomes who may well be willing to upgrade to a better visual experience. It is up to us to give them that opportunity, without any prejudice regarding their budgets. In other words, talk about customized single vision and relaxed vision lenses to every patient you consider a candidate.
Focus on the greatest need. As discussed above, there is a significant population of traditional single vision wearers who aren’t getting clear vision across the entire lens. But in most cases, they’re not likely to complain, because they have grown used to the limitations of their lenses and assume that a better experience is not available. The patients most likely to be experiencing problems are those needing sphere powers above +/- 2.00 or cylinder above -1.50. It’s a good idea to talk to all of these patients about customized single vision.
Identifying the need for relaxed vision lenses is somewhat more subjective. In this case, focus on younger patients who are heavy users of digital devices and suffer from symptoms such as tired eyes, headaches, or neck and shoulder pain. These patients may not associate all of these symptoms with their vision, and they are likely unaware that there is a type of lens that can alleviate the symptoms.
t’s easy to assume that patients are content with the lenses they are wearing now, or that they won’t be willing to pay for something better. But if we make these assumptions, we risk denying patients the benefits of technological progress. (And as we’ve seen, progress in lenses for younger wearers has been significant.) As with so many aspects of vision care, communication is the key to higher patient satisfaction and practice success.■
Jeff Hopkins is an ophthalmic lens and dispensing expert with experience in marketing, education, manufacturing and distribution.













