
By Palmer R. Cook, OD
All horns make noise. Goat horns, giraffe horns and unicorn horns are naturally excluded, but clarinets, coronets, trombones, trumpets, French horns and sousaphones, and even auto horns certainly qualify. Saying, “All horns make noise,” is akin to saying, “All ophthalmic lenses focus light.” This is generally but not completely true.
Another generalization about ophthalmic lenses is, “All lenses perform equally well.” In order to make that generalization work, “through the optical center” must be added. Experienced ECPs know that optical performance in the periphery is where performance problems arise. If you are fitting a -4.00, it really doesn’t matter much from a visual performance standpoint, whether you fit a biconcave lens, a plano-concave, or a meniscus lens. In any configuration (Fig. 1), a lens with the needed power will correct refractive error equally well—as long as the patient only looks through the optical center (OC) and optical axis. The good news is that digital technology is available to relieve problems of away-from-center viewing.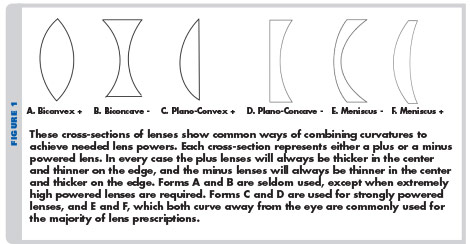
As soon as the patient’s line-of-sight turns away from the optical center (OC), optical goblins, called aberrations, creep in and lens performance begins to deteriorate. At a short distance from the OC, the effect of aberrations can be so minimal that the visual system cannot sense the deterioration in optical performance, but as the line-of-sight moves further into the lens periphery, the effect of aberrations becomes greater. Despite the most strenuous admonitions of optometrists and opticians to be “nose pointers,” humans, being as they are, continue to turn and converge their eyes in the most counterproductive (optically speaking) manner. In other words, although looking through the OC gives the best the lens has to offer and essentially eliminates common aberrations, trying to train patients to only look through the OC of their lenses is not practical.
DEFOCUS
In order not to lose sight of what we are trying to do for our patients, we must address an important aberration of the eye itself: defocus. Defocus is an ocular aberration in which the image of a distant object formed by the cornea and lens (in a non-accommodative state) fails to fall on the retina. This is also called refractive error. Astigmatism is a special condition of defocus in which the amount of defocus varies from meridian to meridian. Defocus is an aberration that we correct by adding optical power to, or by subtracting optical power from, the eye’s optical system. That’s why plus and minus signs are used when writing lens prescriptions.
Assuming the refraction is accurate, defocus should be corrected when the patient looks through the optical center of a single vision lens. The lens power formula the doctor writes usually only gives the power needed to correct the defocus problems of the patient’s eyes. Unless the doctor specifies a lens design that compensates for aberrations, it is up to the person placing the lens order to figure out what lens materials and curvatures will work best. This puts a great deal of responsibility for understanding ophthalmic lens designs on the shoulders of opticians and ophthalmic technicians. Digital technology allows correction (through atoricity) of peripheral aberrations in all major meridians for astigmatics rather than in only one major meridian as in corrected curve technology.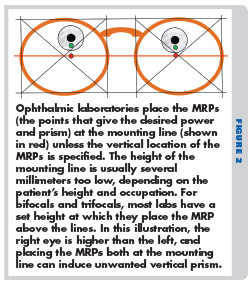 Obviously, the optical center (OC) of the ophthalmic lenses should be positioned so that the patient will view through those points as much as possible. When no prism is prescribed, the optical center is also the Major Reference Point (MRP) of the lens. If the patient has prism prescribed, the MRP is the point that should be so positioned. No matter what power or lens design is used, correctly positioning the MRP is one of the most important factors in minimizing the effect of aberrations.
Obviously, the optical center (OC) of the ophthalmic lenses should be positioned so that the patient will view through those points as much as possible. When no prism is prescribed, the optical center is also the Major Reference Point (MRP) of the lens. If the patient has prism prescribed, the MRP is the point that should be so positioned. No matter what power or lens design is used, correctly positioning the MRP is one of the most important factors in minimizing the effect of aberrations.
We actually spend more time looking downward rather than keeping our lines-of-sight horizontal. When walking, most adults look downward at a point about 17 feet ahead, and we often look downward to view things we are holding or upon which we are working. Therefore, it makes sense to specify the vertical locations, as well as the lateral placement of the MRPs (Fig. 2). The failure to specify these vertical locations is one of the most common and most fundamental errors that are made when ordering lenses.
CHROMATIC ABERRATION
Chromatic aberration is a polychromatic effect in which various colors (wavelengths) of light are refracted or bent to a greater or lesser extent than other colors. It is related to the physical properties of lens materials. Although complicated optical systems can use special compound lens designs called achromats to reduce chromatic aberration, this is not practical for ophthalmic lenses. Reducing the effect of chromatic aberration is largely limited to careful selection of lens materials. Equally important is understanding those factors that make patients more prone to problems related to chromatic aberration (Table 1).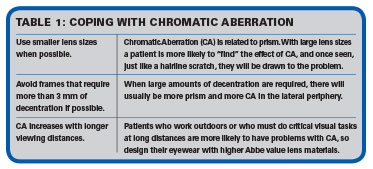
Changing the curvature of a lens cannot change chromatic aberration. Fortunately, the other two common lens aberrations, power error and marginal astigmatism, can be reduced by changing the way the lens is curved or bent. Chromatic aberration becomes troublesome only when the patient is looking through prism. This is true whether the prism is prescribed or induced by looking away from the optical center of the lens.
SEIDEL ABERRATIONS
There are five Seidel monochromatic aberrations found in ophthalmic lenses. Spherical aberration is a condition in which parallel rays from an object entering a large area of a lens are focused at differing distances from the optic axis, depending on how centrally or peripherally they enter the lens. Coma is a condition similar to spherical aberration that refers to ray bundles not centered on the optic axis. Coma causes objects viewed away from the center of the lens in such a way that more peripheral rays are more magnified than rays that are toward the optic axis. Marginal astigmatism (also called oblique astigmatism) is astigmatism created when a small bundle of peripheral light rays strike the peripheral spherical curves of a lens at an angle. Power error (also called curvature of field) is the condition in which the power of the lens changes as the eye turns to view peripheral objects. The fifth Seidel aberration is distortion. This is caused by increased or decreased magnification in the periphery (compared to the magnification in the central area of the lens). It is sometimes referred to as pincushion distortion in the case of plus lenses and barrel distortion in the case of minus lenses.
The pupil limits both spherical aberration and coma, and so they are of little consequence, particularly for pupils of about 5 mm or less. Distortion is curious in that it distorts shapes, but unlike the other Seidel aberrations, it does not cause blur. Properly bending of the lens or using aspheric curves can address the remaining Seidel aberrations, marginal astigmatism and power error.
MARGINAL ASTIGMATISM
Selecting an appropriate base curve can control marginal astigmatism yielding clearer vision through the lens periphery. This is how corrected curve lenses (technology that was developed decades ago) address marginal astigmatism.
Digital technology now produces aspheric curves that can reduce the marginal astigmatism. These curves are flatter than corrected curve designs, and they are produced by lens surfacing equipment that can “fine tune” these aspheric curves to match individual lens prescriptions. This is a considerable improvement over offering base curves in 2 or 3 diopter steps as is required with non-digital production methods.
POWER ERROR
This aberration causes the focus of the lens to fail to fall on the Far Point Sphere when the eye rotates from the straight-ahead position (Fig. 3). When the eye rotates, its dioptric power does not change, but the power of an ophthalmic lens does change when areas of the lens away from the center are measured. This change varies depending on how the lens is curved. Corrected curved lenses have a spherical curvature in each meridian, and by selecting an appropriate base curve, power error can be controlled. Newer digital technology now allows us to make aspheric curves that can control power error and at the same time give us thinner, less steeply curved lenses.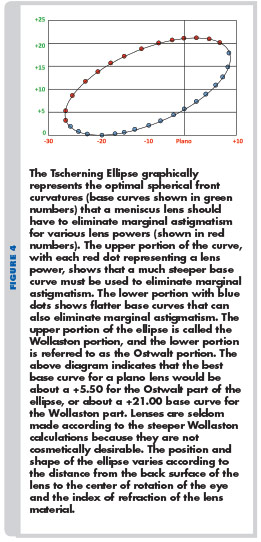 ASPHERIC ADVANTAGES
ASPHERIC ADVANTAGES
Digital lens production permits lens curves that change from the center of the lens to the periphery (aspheric curves). In the case of correcting astigmatism, the amount of asphericity can be modified so that the correction of aberrations can be controlled for both major meridians rather than only one as is done with corrected curve lenses. Even better, digital technology allows the lens curvatures to match the patient’s exact prescription, unlike the older technology, which only corrected for the spherical power and approximated the needed base curve for strong cylinders.
When correcting the common aberrations that affect spectacle lens wearers, lens designers must choose among correcting marginal astigmatism, power error, or an averaging of the two. This is done for a given viewing angle, usually somewhere around 30 to 40 degrees, into the periphery of the lens. If the exact spherical curvature were offered for every prescription and every meridian in accordance with the Tsherning Ellipse (Fig. 4), the result would be lenses that are more steeply curved, but which might have a somewhat larger sweet spot. If digital technology is used to replace the spherical curves with aspheric curves, flatter and thinner lenses result.
Creating patient-pleasing eyewear includes selecting an appropriate lens material, a frame that is mechanically and cosmetically acceptable, and an appropriate lens design. It also helps if the refractive findings are taken correctly. Lens designers assume that when the refractive findings are taken, three conditions will be met: 1. The plane of the test lens is at right angles (“normal”) to the line-of-sight, 2. The line-of-sight is passing through the OCs of the test lenses, and 3. The refracting vertex matches the vertex at which the lenses will be worn. For low power refractive errors, these conditions are less critical, but for stronger powers, the conditions should be met as closely as possible. The refractor’s pinholes can and should be used both for accuracy, and to be sure the patient is tested through the OCs as well as being properly leveled when locating the axis for strong cylinder powers. The refractor apertures should be at the same height as the target chart, and the plane of the chart should be parallel to the test lens plane. If the patient must look up, down or to the side to view the target chart through the refractor, sphere and cylinder errors will be introduced just as wrap and pantoscopic tilt change lens effectivity. Ideally, the refracting vertex should be the same as the vertex assumption of the designer of the lens you plan to use.
KNOWING OUTCOMES
The information provided by manufacturers about their lens designs is sparse. For the most part, manufacturers neither reveal what aberrations they are trying to reduce, nor do they give data on the efficacy of their designs. Some experienced optometrists and opticians tend to feel, over time, that they have fewer complaints with one or another design, and they favor those designs that seem least troublesome. This is a trial-and-error process that is neither efficient, nor is it necessarily very accurate. Others that do post-dispensing follow-ups have a huge advantage. Marginally satisfied patients may not return to complain, and they may simply not ever return. By using some form of follow-up to determine patient response to recently dispensed eyewear, you can rapidly determine which designs work better.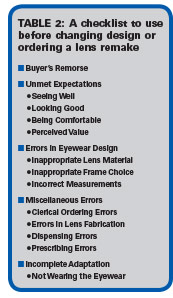 THE BABY AND THE BATHWATER
THE BABY AND THE BATHWATER
Just as you would not want to “throw out the baby with the bathwater,” the problems of patients who have difficulty adapting deserve careful analysis before you blame their difficulties on the lens design. Table 2 lists the most common probable causes for distress over newly dispensed eyewear. It would be wise to carefully consider these categories and subcategories before changing to a different lens design when your patient is distressed about new eyewear. You might also use it as a troubleshooting guide for discussion at your next staff meeting.
Lens manufacturers work hard to produce the best performing products they can, although not all aberrations can be adequately addressed in ophthalmic lens designs. Designs do differ, so if you change lens designs, try to be sure the difference will resolve your patient’s problem. ■
Contributing editor Palmer R. Cook, OD, is director of professional education at Diversified Ophthalmics in Cincinnati, Ohio.













