
PHOTO © PHOTODISC/GETTY IMAGES
Turning an ophthalmic prescription into patient pleasing, high performance eyewear took a giant step forward with the advent of digital lenses. Success with digital demands that dispensers, ophthalmic technicians and other staff members have a working knowledge of digital lenses in order to use this technology most effectively.
One of the most confusing things about digital technology is the terminology. Until there is an industry-wide consensus, we should probably call any lens produced on digital equipment a digital lens. A free-form lens is a digital lens with curvatures generated, not molded, on at least one side and designed for a specific prescription. An individualized lens is a lens with curvatures that are specific for the prescription, the frame as fitted and the patient’s anatomy.
Both free-form and individualized lenses have precisely tailored curvatures for every Rx. Older technology used a handful of curves to cover all Rx powers. Using digital technology effectively requires a careful combining of prescription, lenses and frame.
THE PRESCRIPTION
Individualized and free-form lenses are programmed under the assumption that the doctor examined with the line-of-sight normal (i.e., at right angles) to the test lens’ surfaces, and that the line-of-sight was passing through the optical centers of the test lenses.
For strong prescriptions the power (both sphere and cylinder) may have to be changed before sending the Rx to the lab if the fitting vertex differs from the refracting vertex. Doctors should always note the refracting vertex when the Rx power exceeds about +6.00 or -6.00D.
The Prism Reference Point (PRP) is the optical center of the lens. The distance from the PRP to the reading level in centimeters times the power in each vertical meridian gives the amount of prism for each lens at the reading level. These prism powers should be approximately the same for both right and left lenses. Vertical prism imbalances much over 0.5 or 0.75 prism diopters are often not well-tolerated. Because there can be significant exceptions, the examining doctor should be consulted in cases of excessive imbalance. If the lensometer shows a similar imbalance between the two eyes in the previous eyewear, and if the patient reports he originally did well reading with them, he may tolerate a similar imbalance in the new prescription.
The fitting cross is used industry-wide as the PAL landmark for determining the locations of the other key points of the lens. With digital single vision (SV) lenses, manufacturers may place the optical center of the lens lower than the Distance Reference Point (DRP) to achieve a thinner lens. If this prism thinning is not done, the DRP and the Prism Reference Point (PRP) will coincide as in a conventional SV lens. In either case, performance of the prescription is improved by using atoric, individualized single vision lenses.
THE LENSES
 When lenses are tilted and turned, their optical power changes. The lens designer must cause the digital lathe to generate curvatures that yield the prescription shown by the test lenses, although the eyewear lenses are tilted and turned. In other words, the lenses “as worn” must give the power “as the patient tested.” As worn is another term for individualized.
When lenses are tilted and turned, their optical power changes. The lens designer must cause the digital lathe to generate curvatures that yield the prescription shown by the test lenses, although the eyewear lenses are tilted and turned. In other words, the lenses “as worn” must give the power “as the patient tested.” As worn is another term for individualized.
Astigmatism is a common optical aberration of the human eye. Every lens that corrects astigmatism has optical power that varies from meridian to meridian. Before atoric lenses, curvatures were used to correct for peripheral aberrations (corrected curve lenses), but they could only address the aberrations for the sphere power of the lens. Atoric digital lenses also correct peripheral aberrations for the cylinder power. This creates a larger area of clear, peripheral lens performance around the optical center. Atoricity is an advantage for patients with astigmatism. Many, but not all, digitally produced lenses are atoric.
Lensometers hold lenses so the light flows through at right angles to the lens surfaces. Analyzing an individualized lens or some free-form lenses will not show the prescribed powers. Laboratories deliver these lenses with the compensated power that results when analyzing them with a lensometer. Because patients undergoing adaptation sometimes take their new eyewear elsewhere to “check the prescription,” patients should be told in advance that their individualized or free-form lenses cannot be accurately measured using techniques meant for older style lenses.
THE FRAME
 You should use a centration chart for every digital design you fit. These charts quickly reveal whether the frame of choice can accept the lens design the patient needs. The DRP and Near Reference Point (NRP) allow you to position the lens to read the refractive power for distance and near viewing. The NRP must clearly fall within the eyewire when the centration chart is used, and the lens blank must completely fill the eyewire.
You should use a centration chart for every digital design you fit. These charts quickly reveal whether the frame of choice can accept the lens design the patient needs. The DRP and Near Reference Point (NRP) allow you to position the lens to read the refractive power for distance and near viewing. The NRP must clearly fall within the eyewire when the centration chart is used, and the lens blank must completely fill the eyewire.
If the fitting cross is placed at the center of the pupil with the patient’s head in his “normal” position for straight-ahead distance viewing, he will have to drop his chin somewhat for clear “line-of-sight-level” viewing. Experienced technicians have all developed their own method for fitting cross placement. They either allow the patient to raise his chin as they place the fitting cross, or they have a favorite fudge factor that drops the fitting cross several millimeters. Some successful techs observe the patient after placing the fitting cross and adjust its height as needed. This design technique can increase patient comfort and reduce remakes.
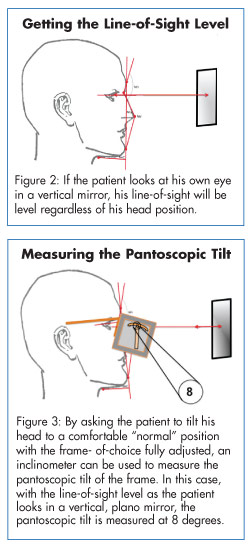
Pantoscopic tilt is the angle at which the lens is rotated from the vertical with the bottom of the lens coming closer to the face from a position of being at a right angle to the line-of-sight. Pantoscopic tilt is sometimes confused with pantoscopic angle, which is the angle the temple makes with the front. The simplest method for measuring pantoscopic tilt is to use an inclinometer and a vertical, plano mirror to establish the patient’s line-of-sight as level.
A basic method for measuring the vertex distance is to first adjust the frame and remove the lenses without disturbing the adjustment. Ask the patient to close his eyes and raise his eyebrows (to stretch the lid tissue a bit). Place a PD rule with the end ground off to the “0” mark through the eyewire at the position of the fitting cross. The vertex distance can then be estimated from above by noting the distance at which the rule passes through the eyewire. One millimeter should be added to account for the thickness of the lid, and a small additional amount can be added if a lens with a steep back curvature is being fitted.
Wrap or face form is the angle at which the lens is rotated in the horizontal from a position of being at a right angle to the line-of-sight. Manufacturers provide instruments or charts for easily measuring this rotation.
When fitting any lens design that separates the distance reference point and the prism reference point, you should treat the lens as though the patient is wearing a prism prescription. In other words, using AR and/or a light tint will improve lens performance. It is likely that fitting individualized lenses will eventually become the rule, and fitting anything else will be very much the exception. ■
To Use Digital Technology Effectively:
- Understand digital terminology, otherwise you will have difficulty making the correct design choices for your patient.
- Be aware that digitally produced lenses can only be as good as their design. The design gives the performance; digital lathes make the design a reality.
- Use digitally produced, individualized lenses for the very best performance. They are tailored to your patient's anatomy, frame and prescription.
- Since there is little definitive information available about results at various refractive levels, select patients in the moderate or higher sphere powers and/or those with 1.50 diopters of cylinder or more to learn how well these lenses really work. Follow up 10 days or so after dispensing with a phone call. The object is to be sure your patient's eyes are responding to the new lens technology. Ask about resolution of the chief complaints. Don't suggest problems. If your patient is having problems he will let you know. Dentists have used follow-up calls successfully for years. They are great practice builders. As you develop the digital lens segment of your practice, you will feel comfortable in expanding to the lower power ranges.
- Never measure for individualized lenses until the frame is properly fitted. Just as refracting to 0.01 diopters is beyond the limits of the human eye's sensitivity, tolerance for measurements can be over-emphasized, but take measurements for individualized lenses as carefully as you can. Anyone who is able to take a PD without a pupilometer should be able to take satisfactory measurements for individualized lenses easily.
- When fitting free-form or individualized lenses with prism, move the Fitting Cross 0.3 mm per diopter of prism in the direction of the apex of the prism. This will allow better alignment of the corridors and the DRP and NRP. If both lateral and vertical prism is present, the Fitting Cross displacement must be according to the amount and direction of the resultant prism. Your lab can help with such calculations.
- Digital single vision designs are available in both free-form and individualized designs. Prism thinning is available and should be considered if the MRP placement is so high that the lens will be excessively thick at the top for plus lenses and at the bottom for minus lenses. If prism thinning is required, the PRP should be at or near the mounting line, and it should be at the same level for both lenses. Measuring the fitting heights, taking accurate PDs and other required measurements if the SV lenses are individualized is just as important for digital SV lenses as it is for PALs.
Palmer R. Cook, OD, is director of professional education at Diversified Ophthalmics, Cincinnati, Ohio.













