Over the past year, researchers have continued to refine and expand our understanding of glaucoma and its treatment options. Here are some selected highlights from this year's new data. (Studies were done without commercial support unless otherwise noted.)
Improving Surgical Outcomes
With anti-VEGF (vascular endothelial growth factor) drugs making headlines, more researchers are studying ways in which these drugs might be useful in the treatment of glaucoma. One such study, a prospective, non-randomized, open-labeled pilot study conducted by researchers at
In the study, 39 eyes with primary open-angle glaucoma, normal-tension glaucoma or exfoliation syndrome underwent a trabeculectomy augmented with mitomycin or 5-FU between November 1997 and October 2006. A subconjunctival injection of bevacizumab (1 mg) was administered proximal to the bleb at the earliest sign of vascularization. If excessive vascularity of the bleb was still observed, the injection was repeated.
Ultimate-ly, 23 eyes had one injection, nine eyes received two injections, and seven eyes received three injections. The mean pre-injection IOP was 17.8 ±6.4 mmHg. Intraocular pressure, bleb vascularity and fibrosis were evaluated weekly until the bleb was stable; re-evaluations were done monthly.
Findings included:
• Twenty-four of the 39 eyes displayed a detectable decrease in the vascularity of the bleb.
• There was no evidence of any side effects from the injection.
• One month post-injection, the mean IOP was 14 ±4.5 mmHg, a statistically significant decrease (p= 0.001). After the first month the IOP measurement gradually increased, but it never exceeded the pre-injection/ post-trabeculectomy level.837
In a second VEGF-related study, researchers at the University of Florida-Jacksonville investigated the possibility that the ciliary body is a source of VEGF in patients with neovascular glaucoma. (The study authors had previously reported increased levels of VEGF protein in the aqueous humor of eyes with uncontrolled neovascular glaucoma.)
Researchers processed 12 human eyes enucleated for uncontrolled NVG for immunodetection of VEGF protein and hybridization in situ to localize its mRNA.
Findings included:
• A strong immunoreaction—15 times that of age-matched normal eyes—was observed in the nonpigmented ciliary epithelial cells of NVG eyes.
• While minimal or no staining for VEGF mRNA was detected in ocular tissues of control eyes, eyes with NVG showed strong staining in the nonpigmented ciliary epithelium—six times that of control eyes.
• VEGF mRNA expression was also observed in the ganglion cell, inner nuclear and outer nuclear layers of the retina in eyes with rubeosis iridis.
The study authors note that an extraretinal source for the synthesis of VEGF in eyes with uncontrolled NVG may account for increased levels of VEGF protein in the aqueous humor, and may explain why pan-retinal photocoagulation doesn't induce regression of iris neovascularization in all patients with venous thrombosis and/or diabetic retinopathy. It may also provide a rationale for ablating the ciliary body as a treatment for NVG.5914
Working with Shunts
A number of studies focused on the safety and efficacy of shunts, including the Ex-PRESS shunt. In one, researchers at the University of Tennessee Health Sciences Center and the Dean McGee Eye Institute in
During a mean follow-up period of 17 months (range: three to 36 months):
• IOP averaged 14.7 ±7.1 mmHg at six months (p<0.001); 15.2 ±7.9 mmHg at nine months (p<0.001); and 15.2 ±7.9 at one year (p<0.001) postoperatively.
• The number of glaucoma medications was significantly reduced.
• The success rate, as defined above, was 89 percent at six months, 87.3 percent at nine months, and 84.9 percent at one year postoperatively.
No erosion of the conjunctiva over the device occurred in this series, although the study authors note that five patients (1.7 percent) developed obstruction of the lumen of the Ex-PRESS implant, which was successfully treated with the Nd:YAG laser.819
Another study, conducted at the 
The primary outcome measure was the incidence of hypotony (IOP <5 mmHg) in the postoperative period (four weeks to one year after surgery). They found that in the uveitic group, 10 of the 13 eyes (77 percent) had documented hypotony at some point in the postoperative course—a higher incidence than previously reported in the literature. In contrast, only one of the 19 eyes in the non-uveitic group (5 percent) had hypotony (p<0.0001).
The authors conclude that hypotony is more common following BGI surgery in uveitic eyes, which should aid clinicians in preoperative planning and postoperative management.3954
Clinical Risk Factors
A study conducted at the University of California-San Diego attempted to determine whether long-term IOP fluctuations are a risk factor for conversion from ocular hypertension to glaucoma. The study included 105 untreated patients with ocular hypertension who were followed as part of the Diagnostic Innovations in Glaucoma Study (DIGS). The subjects had IOP greater than 22 mmHg in both eyes, normal visual fields and normal optic discs as evaluated by stereophotograph assessment.
Twenty-four patients (23 percent) developed glaucoma (defined as reproducible visual field loss or progression of optic-disc damage) during a mean follow-up time of seven years (84.7 ±46.2 months). Mean IOP was calculated as the arithmetic mean of IOP over the course of all visits for non-converters, and visits up to the beginning of progression for those who converted. IOP fluctuation was calculated as the standard deviation of IOP at these visits. Multivariate models adjusted for age, central corneal thickness, vertical cup/disc ratio and pattern standard deviation.
The data showed that while mean IOP during follow-up was a significant risk factor for progression in untreated ocular hypertensive subjects, IOP fluctuation was not, in either univariate or multivariate analysis. Converters' mean IOP fluctuation was 2.76 ±1.16 mmHg; non-converters mean IOP fluctuation was 2.63 ±0.86 (p=0.548).851
Myopia has been proposed as a risk factor for OAG, but researchers at the Doheny Eye Institute and
The data showed that myopes were significantly more likely to have OAG (8.1 percent) than non-myopes (3.7 percent, p<0.0001). This association remained after adjusting for severity of nuclear opacification (p=0.0003). After adjusting for covariates, persons with longer axial length had a higher risk of having OAG compared to those with shorter axial length (p<0.0001). The authors conclude that myopia and longer axial length are both risk factors for OAG in adult Latinos.1557
Managing IOP
A randomized, prospective study conducted at Bascom Palmer in
Forty-three patients and normal volunteers ages 18 to 75, with no history of prior intraocular surgery, laser therapy or disease that might affect the accuracy of the study's measurements, were randomly divided into two groups. One group had the right eye measured in the sequence pachymetry-tonometry-pachymetry, followed by the left eye measured in the sequence tonometry-pachymetry-tonometry. The other group also started in the right eye, but with the sequences switched. A single examiner, using a Goldmann Tonometer and the Pachette Ultrasound Pachymeter, sequentially performed the measurements, less than one minute apart.
The study found:
• In the tonometry-first eye, 34 of 43 eyes showed a change in IOP no greater than 1.5 mmHg. However, after pachymetry testing, eight of the 43 showed an IOP decrease of at least 2 mmHg, and one eye showed a pressure increase greater than 2 mmHg.
• In the pachymetry-first eye, the corneal thickness following tonometry remained within 5 µm for 38 of the 43 participants and within 10 µm for all participants.
• IOP measured after pachymetry was a mean of 0.9 mmHg less than IOP measured before pachymetry (p=0.000002). In contrast, when pachymetry was measured after applanation the result was only 0.1 ±3.2 µm less than when measured before applanation (p=0.424).1257
A retrospective chart review of 224 patients with glaucoma or ocular hypertension conducted at the
Subjects included 136 females and 175 African Americans; mean age was 66. CCT was measured with ultrasonic pachymetry before treatment. Subjects were placed into three groups: Group one had a CCT less than 520 µm (n=93); group two's CCT was between 520 and 559 µm (n=83); and group three's CCT was thicker than 560 µm (n=48). Then, subjects underwent a monocular trial with alpha agonists, beta-blockers, carbonic anhydrase inhibitors or prostaglandin analogues. (The study medication was the first IOP-lowering drop ever used by 169 of the patients.)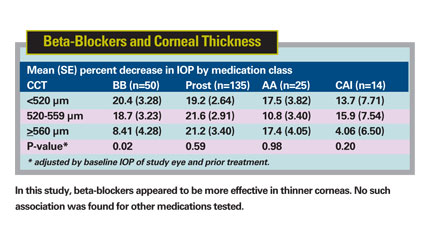
IOP was measured using Goldmann tonometry at the beginning of the trial and one to 17 weeks after the initiation of treatment. (To minimize the effect of diurnal fluctuation on IOP, the percentage change in IOP in the treated eye was calculated as the difference in IOP from baseline between the treated and the contralateral eye, divided by the baseline IOP of the treated eye.)
Eyes in which the study medication was added to previous treatment had a smaller IOP reduction than eyes that were not treated before. The mean percentage decrease in IOP in 169 previously untreated eyes was 22.3, as compared to 15.2 in 55 previously treated eyes (p=0.005).
Overall, IOP change was not associated with CCT; the percentage decrease in IOP was 21.1 ±1.71 in group one, 21.2 ±1.81 in group two, and 18.7 ±2.38 in group three (p=0.66). However, analysis by medication class showed that beta blockers were more effective in thinner corneas (p=0.02). No such association was found for prostaglandins, AAs or CAIs.1279
Imaging and Perimetry
Data from a foundation-supported study conducted at the
Researchers analyzed the neuroretinal rim areas of each quadrant of the right eye, and noted the percentages of eyes showing different patterns of rim area quadrant orders. The data showed that the average rim area, in descending order was inferior, nasal, superior and temporal (INST). (The percentage of eyes with the thickest rim area in each location is shown in the table below.) By frequency, the percentage of eyes following the various rules were: NIST , 33 percent; INST, 21 percent; ISNT, 18 percent; NSIT, 10 percent; SINT, 6 percent; and SNIT, 3 percent. The study authors note that vascular structures in the nasal quadrant likely contributed to these results.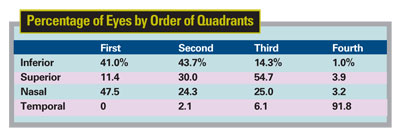
Although the rank order of HRT 3 rim area data doesn't follow the ISNT rule (the NIST and INST rules were more common), the authors believe that the order of rim area may be helpful for determining optic nerve health, as in the finding that the temporal rim area was smallest in 92 percent of these normal eyes.3314
A study conducted at multiple sites in
Eyes with ANA (Shaffer grade 2) were imaged under light and dark conditions; angle opening distance at 500 µm was recorded using each device for superior and inferior angles. SL-OCT and UBM images and gonioscopy under dark conditions were assessed for iridotrabecular contact.
The data showed:
• In both superior and inferior angles, angle opening distance at 500 µm was less when measured by UBM than SL-OCT. Differences between instruments were highly significant in the inferior angle in light and dark conditions (all p<0.0001).
• In the superior angle, a highly significant difference was seen in light (p=0.002), but not in dark (p=0.153).
• When controlled for light and dark conditions, differences remained highly significant for superior (p= 0.006) and inferior angles (p<0.001).
• Specifying UBM as the gold standard for iridotrabecular contact, SL-OCT had 80 percent sensitivity and 87 percent specificity in the superior angle; sensitivity was 100 percent with 62 percent specificity in the inferior angle. Gonioscopy had 95 percent and 85 percent sensitivity in the superior and inferior angles, respectively; specificity was 67 percent in both locations.
The authors note that factors influencing the appearance of the angle include method of assessment, the software used to process images, illumination, patient posture and contact during the procedure. SL-OCT appears to underestimate the frequency of iridotrabecular contact.873
Researchers in Singapore, Baltimore and London conducted an observational cross-sectional study involving 502 subjects with no previous ophthalmic problems recruited from a community clinic in Singapore, to see whether gonioscopy or anterior segment optical coherence tomography (AS-OCT) was better at detecting angle closure. (One study author is a consultant for Carl Zeiss Meditec.)
Clinicians obtained AS-OCT images of the four quadrants of the right eye in dark conditions; images were evaluated by a second masked examiner. Gonioscopy was performed in dim lighting by a masked examiner; an angle quadrant was classified as closed if the posterior trabecular meshwork could not be seen (Shaffer grade 0 or 1). With AS-OCT, a closed angle quadrant was defined by the presence of any contact between the iris and angle wall anterior to the scleral spur.
The data showed:
• AS-OCT detected a closed angle in at least one quadrant in 298 eyes (59 percent); gonioscopy detected this in 161 eyes (32 percent) (p<0.001). Overall agreement was fair (kappa= 0.37).
• The frequency of closed angles in each quadrant detected by AS-OCT and gonioscopy was: superior, 246 (49 percent) vs. 143 (28 percent); inferior, 199 (40 percent) vs. 104 (21 percent); nasal, 89 (18 percent) vs. 67 (13 percent); and temporal, 60 (12 percent) vs. 89 (18 percent).
• Of the 129 quadrants that appeared closed on gonioscopy but open on AS-OCT, 89 percent (115) displayed an "over the hill" iris configuration (below, left). Of the 335 quadrants that were open on gonioscopy but closed on AS-OCT, 75 percent (250) showed low irido-angle contact on AS-OCT (below, right).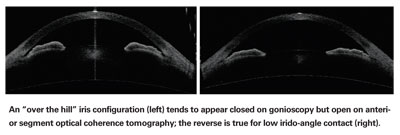
The authors conclude that AS-OCT identified more eyes as having angle closure than gonioscopy, particularly in the superior/inferior quadrants, and variations in iris profile and level of irido-corneal contact may account for some of these differences.1975
A multicenter investigation, using information gathered during the African Descent and Glaucoma Evaluation Study and the Diagnostic Innovations in Glaucoma Study, compared the structure of the optic nerve and RNFL in healthy participants of African and European descent (AD, n= 190; ED, n=194). Many of the study authors were affiliated with Carl Zeiss Meditec or Heidelberg Engineering.
The study included 384 eyes (one per subject) that had normal fundus exams, visual fields and optic disc stereophotos, and IOPs <22 mmHg. Optic nerve topographic information was obtained using CSLO and OCT imaging; RNFL thickness measurements were obtained using CSLO, OCT and SLP imaging.
The data (see chart, below) showed that individuals of African descent had larger optic disc and cup areas, deeper cups and a larger neuro-retinal rim than those of European descent. However, after adjustment for differences in disc area, these differences were not significant. The authors also noted that the Moorefield Regression Analysis (MRA) performed with high specificity (99.4 percent AD, 100 percent ED), while the Glaucoma Probability Score showed a lower specificity in the AD group (83 percent AD, 89 percent ED; p=0.021)
The authors conclude that the morphological differences need to be taken into account when interpreting results of diagnostic imaging in differing demographic groups, and that diagnostic methods that take differences in optic disc area into account, such as MRA, have a higher specificity in individuals of African descent.3315
In a study conducted in
Researchers measured refractive error, axial length and corneal power, and measured thicknesses of the fovea and the peripapillary RNFL in all subjects using OCT. A manifest refraction between 0 and -2 D was classified as emmetropia and low myopia (group one, 45 eyes); between -2 and -5 D was classified as moderate myopia (group two, 43 eyes); more than -5 D was classified as high myopia (group three, 28 eyes). The data showed:
• There were significant differences in thickness of the fovea among the groups: 142.16 ±8.99 µm in group one; 153.58 ±17.63 µm in group two; and 158.86 ±11.93 µm in group three.
• The average thickness of the peripapillary RNFL was 113.29 ±10.80 µm in group one, 103.85 ±14.48 µm in group two and 100.74 ±9.15 µm in group three. There was a statistically significant difference between group one and the other groups (p<0.05).
• As axial length increased, the thickness of the fovea also increased, yet the thickness of the peripapillary RNFL decreased (p<0.05).
• There was no correlation between corneal power and thickness of the fovea, or between corneal power and thickness of peripapillary RNFL.
The study authors note that given these correlations to myopia, care should be used when interpreting the results of OCT scans in the clinic.1011
Protecting Your Patients
Because caffeine consumption has been positively associated with elevated IOP in open-angle glaucoma patients, researchers in
During the follow-up period, researchers identified 856 self-reported POAG cases that were confirmed with medical record review. Overall, caffeine consumption was not associated with risk of POAG, but the data indicated that very high consumption significantly increased risk. Those consuming six or more cups a day had a 1.71-fold increased risk compared to those not consuming any coffee [p for linear trend = 0.03]. Associations were more adverse in relation to POAG with elevated IOP, but no associations with tea intake were observed.4341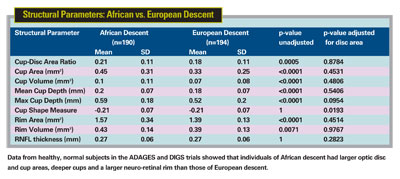
Researchers at
Driving performance was tested over a 10-km route incorporating 55 maneuvers through residential and business districts. Testing was conducted by a professional driving instructor and assessed by an occupational therapist experienced in driving rehabilitation, neither of whom had any knowledge regarding the status of the participants.
The study found no significant difference between glaucoma patients and controls in the number of maneuvers correctly executed, or overall rating of performance. However, glaucoma patients were more than five times more likely to make one or more critical errors, and in 80 percent of cases the critical error was failure to yield to a pedestrian. (A Humphrey Field Analyzer mean deviation of less than -5 dB in the worse eye was strongly associated with such errors.)4449
A study conducted in
In the first, Dark Agouti rat eyes injected with intravitreal staurosporine (SSP) were randomly assigned to five different treatment groups of 18 rats each; topical CoQ10 0.1% x1 or x2, topical CoQ10 0.05%, or carrier/ saline control. Treatments were given four hours or 30 minutes before, or one hour after SSP administration under general anesthesia. Eyes were imaged in vivo via detection of apoptosing retinal cells (DARC), with results confirmed histologically.
In the second model, the most effective dosing regimens were compared to control in a chronic ocular hypertension rat model (n=10) with DARC imaging at three weeks after IOP elevation. The data showed that:
• CoQ10 0.1% significantly reduced RGC apoptosis compared to CoQ10 0.05% (p<0.05) and carrier (p<0.05) in the SSP model.
• The most effective timing of the treatment application was one hour after SSP administration. CoQ10 0.1% administered at this time significantly inhibited the development of RGC apoptosis in vivo at three weeks in the OHT model (p<0.05).
The study authors note that CoQ10 0.1% demonstrated a neuroprotective effect on both SSP-induced and OHT-induced RGC apoptosis in vivo, and that its effectiveness in eyedrop form is particularly exciting.4369
Dr. Netland is the Siegal Professor, director of glaucoma and vice chair for academic affairs in the Department of Ophthalmology at the Hamilton Eye Institute, University of Tennessee Health Science Center,











