MILLIONS OF AMERICANS suffer from hematological disorders, which can cause significant ocular complications in our patients. In fact, ocular manifestations can be the presenting signs or symptoms in up to 90% of patients depending on the underlying hematological disorder.1 Here we discuss the retinal findings of anemic retinopathy, sickle cell retinopathy, leukemic retinopathy, and lymphoma, as well as treatment options currently available.
Anemic Retinopathy
The anemias occur when the level of healthy red blood cells (RBCs) or hemoglobin (an iron binding, oxygen-carrying protein within the red blood cells) is too low. Anemia can be due to nutritional problems such as an iron deficiency, vitamin deficiency or folate deficiency. Iron deficiency is the most common type of anemia. A deficiency of vitamin B12 is known as pernicious anemia. Other causes of anemia include blood loss, inadequate production of red blood cells (aplasic anemia) or increased destruction of red blood cells (hemolytic anemia) that may present lifelong health problems.
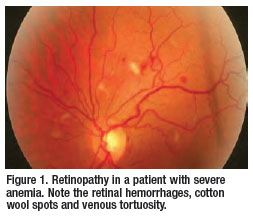 Retinopathy in patients with anemia is
well documented. Common findings
include hemorrhages that can present at
all levels of the retina and choroid,
Roth’s spots, exudates, cotton wool spots,
retinal edema and venous tortuosity
(Figure 1). Roth’s spots or white centered
hemorrhages are typically associated with
bacterial endocarditis, however the association
is not exclusive, since they occur
in diverse conditions including anemia.
The white center could represent focal
ischemia, inflammatory infiltrates, infectious
organisms, fibrin and platelets, or
an accumulation of neoplastic cells.2 The
exact pathophysiology of anemic
retinopathy is not completely understood.
However, it seems to be related to
retinal hypoxia, venous stasis, angiospasm
and increased capillary permeability.3
Anemic retinopathy is most likely to
occur in patients with severe anemia or
when thrombocytopenia, a disorder of
low platelets, is coexistant.4 The ocular
changes found in anemic retinopathy
are nonspecific and may closely resemble
diabetic or hypertensive retinopathy.
5
Retinopathy in patients with anemia is
well documented. Common findings
include hemorrhages that can present at
all levels of the retina and choroid,
Roth’s spots, exudates, cotton wool spots,
retinal edema and venous tortuosity
(Figure 1). Roth’s spots or white centered
hemorrhages are typically associated with
bacterial endocarditis, however the association
is not exclusive, since they occur
in diverse conditions including anemia.
The white center could represent focal
ischemia, inflammatory infiltrates, infectious
organisms, fibrin and platelets, or
an accumulation of neoplastic cells.2 The
exact pathophysiology of anemic
retinopathy is not completely understood.
However, it seems to be related to
retinal hypoxia, venous stasis, angiospasm
and increased capillary permeability.3
Anemic retinopathy is most likely to
occur in patients with severe anemia or
when thrombocytopenia, a disorder of
low platelets, is coexistant.4 The ocular
changes found in anemic retinopathy
are nonspecific and may closely resemble
diabetic or hypertensive retinopathy.
5
Anemic retinopathy may also be a secondary manifestation of other systemic diseases such as cancer, infection or autoimmune disorders. Therefore, in addition to ordering a complete blood count (CBC w/differential), other appropriate medical testing may be necessary. In regards to the management, anemic retinopathy is reversible with correction of the anemia.
Sickle Cell Retinopathy
The sickle cell hemoglobinopathies are an inherited group of disorders that are due to a structurally abnormal beta hemoglobin chain subunit. The result is formation of crescent-like, or sickle shaped, red blood cells in response to decreased oxygen concentration or other physiological stresses. Sickle cell disease is one of the most prevalent genetic disorders in the United States and it predominately affects individuals of African descent and Mediterranean ancestry. Approximately 10% to 14 % of North American blacks are affected with one of the four known variants of sickle cell.6,7
 The four common variants include
sickle cell anemia (SS), sickle-hemoglobin
C disease (SC), sickle beta- thalassemia
and sickle cell trait (AS).
Individuals with sickle cell trait inherit
one normal hemoglobin and one sickle
hemoglobin-S, resulting in the AS genotype.
The sickle cell trait is the most
common of the sickle hemoglobinopathies,
and it affects approximately
8% to 10% of
the black population
(AS).8 To
confirm the disease,
the patient
may require a
hemoglobin
electrophoresis
or DNA analysis.
The four common variants include
sickle cell anemia (SS), sickle-hemoglobin
C disease (SC), sickle beta- thalassemia
and sickle cell trait (AS).
Individuals with sickle cell trait inherit
one normal hemoglobin and one sickle
hemoglobin-S, resulting in the AS genotype.
The sickle cell trait is the most
common of the sickle hemoglobinopathies,
and it affects approximately
8% to 10% of
the black population
(AS).8 To
confirm the disease,
the patient
may require a
hemoglobin
electrophoresis
or DNA analysis.
The ocular complications of sickle cell disease are caused by microvascular occlusion secondary to the sickling of red blood cells. Retinal hypoxia, ischemia, infarction, neovascularization, and fibrovascularization may result from the microvascular occlusion.9 The retinopathy can be divided into non-proliferative and prolifertive changes (Table 1). Although neovascularization may be seen at the optic disc and the macula, proliferative sickle retinopathy is primarily a peripheral retinal disease that can lead to severe vision loss. Proliferative retinopathy is more characteristic of patients with SC and SB thalassemia disease than the more severe systemic form of sickle cell anemia.10
Additional retinal complications of sickle cell disease include sickling maculopathy, central retinal artery occlusion (CRAO), branch retinal artery occlusion (BRAO), epiretinal membrane, ischemic optic neuropathy, development of optociliary shunt vessels, and choioretinal infarctions.11 The presence of a retinal artery occlusion in black patients under the age of 40 should raise the consideration of underlying sickle hemaglobinopathies. Although rare, retinopathy can occur in patients with sickle cell trait in the absence and presence of concomitant systemic disease, such as diabetes or hypertension.12
Patients with non-proliferative retinopathy should be followed periodically according to the level of involvement. For proliferative retinopathy, the aim is to prevent ischemic complications, particularly vitreous hemorrhages and retinal detachments. Treatment options include the use of diathermy, cryotherapy, and laser photocoagulation.13 Recent studies have investigated the role of pigment epithelium-derived factor (PEDF) and vascular endothelial growth factor (VEGF) in the progression of neovascularization. Siqueira and associates demonstrated retinal neovascularization regression with intravitreal Avastin (bevacizumab, Genentech) injection.14 Additional studies are necessary however, to demonstrate the reliability of anti- VEGF use in the management of proliferative sickle cell retinopathy.
Leukemic Retinopathy
Leukemia is defined as a neoplastic blood disorder characterized by the overproduction of abnormal white blood cells. Leukemia can be divided into two types; myelogenous and lymphocytic. Leukemia is further divided into acute myelogenous leukemia (AML), acute lymphocytic leukemia (ALL), chronic myelogenous leukemia (CML) or chronic lymphocytic leukemia (CLL). Approximately 50% or more of all leukemias manifest some form of ocular involvement.15,16
The ocular complications of leukemia may be due to a direct involvement by leukemic infiltrates or secondary to concomitant anemia or thrombocytopaenia. 17 Leukemic retinopathy is a common manifestation of leukemia and is found in both the acute and chronic forms. Features of leukemic retinopathy include multiple preretinal and intraretinal hemorrhages that are most commonly found in the posterior pole. Other features include Roth’s spots, cotton wool spots, exudates, retinal venous tortuosity, perivascular sheathing, and neovascularization. Roth’s spot hemorrhages may represent small areas of retinal leukemic infiltration or plateletfibrin deposits. Retinal lesions such as peripheral neovasularization or sea fans neovascularization (reminiscent of sickle cell retinopathy) may develop in patients with chronic leukemia and are thought to occur as a result of peripheral nonperfusion and ischemia from the hyperviscosity. 15 Serous retinal detachments and various other retinal anomalies have been reported, as well as pallor and swelling of the optic nerve, which indicate optic nerve infiltration.15
In pathological studies, the choroid is the most commonly affected ocular structure. Choroidal masses lead to a disruption of the retinal pigment epithelium which result from decreased blood flow to the choriocapillaris.16 In some cases a serous or exudative retinal detachment may ensue.
Leukemic retinopathy usually is not treated directly. Systemic treatment involves the use of chemotherapy, immunotherapy, and radiotherapy. Intraocular leukemic infiltrate is best treated with chemotherapy that is appropriate for the type and stage of leukemia. External-beam radiation may be applied to lesions of the optic nerve or orbit. The presence of leukemic infiltration is usually a poor prognostic indicator.18
Lymphoma Associated Retinopathy
Lymphomas are a diverse group of cancers of the lymphatic system that comprise 3% to 4% of cancers diagnosed annually.19 Hodgkin’s disease is the most common form of lymphoma; all other lymphomas are termed non-Hodgkin’s lymphomas. Hodgkin’s lymphoma follows a more predictable pattern of growth, and its spread is more limited than non-Hodgkin’s lymphomas. The characteristic pathologic abnormality is a polycellular infiltrate made up of giant (Reed-Sternberg) cells that are fibrotic and necrotic in nature. Orbital involvement is a rare complication of Hodgkin’s disease, whereas non- Hodgkin’s is the most common type of ocular lymphoma.
Ocular abnormalities associated with lymphoma have been divided anatomically into a vitreoretinal and uveal form. The vitreoretinal form is associated with primary central nervous system non- Hodgkin’s lymphoma (PCNSL) and is typically a large B-cell tumor. In contrast, the uveal form is associated with systemic non-Hodgkin’s lymphoma. Involvement of the uveal tract presents as a non-resolving uveitis, diffuse choroidal infitiltration, or exudative retinal detachment. The characteristic retinal finding is a low-lying, yellow-towhite mass deep to the sensory retina. They may even appear as single, multiple, confluent, or discrete punctate lesions that may involve all layers of the retina.20 Retinal phlebitis and the presence of cotton wool spots have been reported as initial clinical findings in Hodgkin’s disease.
Treatment options for lymphoma include observation, involved-field radiation, subtotal lymphoid radiation, chemotherapy with or without radiation, and bone marrow transplant. Newer biologic therapies are also being investigated for the treatment of lymphoma.
Conclusion
Hematological disorders affect millions of Americans and represent a major public health concern due to the potential for significant morbidity and mortality. The retinal findings associated with the various hematological disorders necessitate an immediate comprehensive medical evaluation. The optometric physician may play a crucial role in the diagnosis and management of these disorders.
References
- Lanf GE, Spraul CW, Lang GK. Ocular manifestation of hematological diseases. Klin Monatsbl Augenheik 1998;212: 419-27.
- Kaur B, Taylor D. Fundus hemorrhages in infancy. Surv Ophthalmol 1992;37:1-17.
- Loewenstein JI. Retinopathy associated with blood anomalies. In: Jakobieck F (ed). Clinical Ophthalmology. Revised ed. Philadelphia: J.B. Lippincott Company, 1995;3(85): 995-1000.
- Carraro MC, Rossetti L, Gerli GC. Prevalence of retinopathy in patients with anemia or thrombocytopenia. Eur J Haematol 2001;67:238-44
- Weiss LM. Anemic Retinopathy. Pa Med 1966 Jun;69(6):35-6.
- Motulsky AG. Frequency of sickling disorders in U.S. blacks. N Engl J Med 1973;288:31-3.
- Myerson RM, Harrison E, Lohmuller HW. Incidence and significance of abnormal haemoglobins. Am J Med 1959;26:543.
- Stephen RF. Proliferative sickle cell retinopathy: the disease and a review of its management. Ophthalmic Surgery 1987;18:222-31.
- To KW, Nadel AJ. Ophthalmologic complications in hemoglobinopathies. Hematol Oncol Clin North Am 1991 Jun;5(3):535-48.
- Goldberg MF. Natural history of untreated proliferative sickle retinopathy. Arch Ophth 1971;85(4):428-37.
- Roy MS, Rodgers GP, Noguchi CT, Schechter AN. Retinal signs in sickle cell anemia. Eye 1999;4(6):862-4.
- Welch RB, Goldberg MF. Sickle-cell hemoglobin and its relation to fundus abnormality. Arch Ophthalmol 1970;84:485-90.
- Seiberth V. Trans-scleral diode laser photocoagulation in proliferative sickle cell retinopathy. Ophthalm 1999;106(9):1828-9.
- Siqueira C, Costa RA, Scott IU, et al. Intravitreal bevacizumab (Avastin) injection associated with regression of retinal neovascularization caused by sickle cell retinopathy.
- Miller NR, Walsh FB, Hoyt WF, Newman, NJ. Leukemias/Lymphomas. In: Walsh and Hoyt’s Clinical Neuro- Ophthalmology. Philadelphia: Lippincott Williams and Wilkins, 2005:1613-30.
- Reddy, SC, Jackson N, Menon BS. Ocular Involvement in Leukemia study of 288 cases. Ophthalmologica 2003; 217:441-5.
- Schachat AP, Markowitz JA. Ophthalmic manifestation of leukemia. Arch Ophthalmol 1989;107:697-700.
- Steidl S, Hartnett ME. Leukemia; in Clinical Pathways in Vitreoretinal Disease. Thieme, 2003, 183.
- Sbeity MH, Coupland S, Loeffler KU. High-grade malignant Bcell lymphoma of the retina in a patient with concomitant gastric MALT lymphoma. Graefe Arch Clin Exp Ophthalmol 2007;245(3):448-50.
- Cho HS, Yoon YH. Rapidly developing cotton-wool spots as the first manifestation of systemic non-Hodgkin’s lymphoma. Retina 2003;23(6):877-9.











