Musculoskeletal conditions are the most frequent cause of physical disability in the developed world.1 These pain-associated conditions are comprised of more than 150 various diseases and syndromes (e.g., osteoarthritis, rheumatoid arthritis, tendonitis, bursitis, carpal tunnel syndrome) and are extremely common.1 The burden caused by these conditions is predicted to further increase with the aging of baby boomers. In the next 25 years, it is expected that the number of geriatric patients with arthritis will double to 41 million, and osteoarthritis is expected to be the fourth leading cause of disability by 2020.2,3 But arthritis does not always present as an isolated condition, and clinical signs and symptoms may overlap with other musculoskeletal disorders and comorbidities.
It is common for the primary care practitioner to be consulted for hand and wrist complaints related to musculoskeletal disorders, such as pain and loss of function, especially in seniors.4 While often attributed to osteoarthritis at the thumb, carpal metacarpal (CMC) joint pain, especially acute pain, should never be attributed to normal aging alone. A recent study found that among 267 participants with a mean age of only 49.3 years, the three most frequently recorded diagnoses were osteoarthritis, tenosynovitis, and nerve entrapment (e.g., carpal tunnel syndrome); 74% of patients were female.4 These primary care patients reported pain and reduced function.4 Findings were in line with our understanding that musculoskeletal aging is associated with chronic conditions that impact heavily on the surging geriatric population with regard to functional and economic burden.2 One review of the literature looked at musculoskeletal epidemiology related to aging and found that over 50% of seniors in the United States reported joint symptoms that were chronic in nature.2
Scientists believe it is through research that clinicians can better understand significant chronic conditions that alter the lives of many seniors.2 The researchers stress that the fast-growing geriatric population will require additional clinical study and greater intervention in order to delay or prevent an enormous burden of disability among the elderly related to very common musculoskeletal conditions of aging.2 This article will address tendonitis and tenosynovitis, and will focus on de Quervain's tenosynovitis, also referred to as de Quervain's syndrome. Concise overviews of osteoarthritis and carpal tunnel syndrome in the elderly may be found in the literature.5,6
Tendonitis and Tenosynovitis
A tendon is a fibrous cord of connective tissue that is continuous with the fibers of a muscle and attaches it to bone or cartilage.7 Tendons provide the elasticity and strength that is required to transmit forces of muscle to bone.8 In order to assist with gliding, certain tendons (e.g., the extensors and long abductors of the thumb) are covered with a lining, or sheath, of synovium.8 Inflammation of any part of the tendon is referred to as tendonitis; tenosynovitis is the specific term used when inflammation of the tendon sheath occurs.8,9 Chronic, repetitive overuse of the tendon, acute overload of the tendon, direct injury to the tendon (e.g., microtrauma), and the aging process are the most common causes of tendonitis.8,10 The elderly are at risk for tendonitis secondary to age-related changes in the structure of connective tissue; these changes may also provoke low energy-level tendon rupture.8 Tenosynovitis may also be a manifestation of systemic inflammatory disease (e.g., rheumatoid arthritis), crystalline deposition diseases (e.g., gout), and infection.8,10-12 The structure of the tendon undergoes continuous alteration, including resolution of inflammation in the acute phase and scar formation and remodeling; these stages occur over weeks to months with restriction of motion secondary to scarring.8,9 Furthermore, due to these tendon alterations and subsequent to symptom resolution, there is vulnerability for tendon injury secondary to recurrent, repetitive activity, even long after the initial injury.8
Signs, Symptoms, and Diagnosis of De Quervain's Tenosynovitis
In de Quervain's tenosynovitis, the first dorsal compartment is thickened, raising the skin and creating a prominence at the radial styloid--that is, the tendon sheath of the thumb-side of the wrist becomes inflamed and swollen, which ultimately restricts movement of the tendon and causes pain and discomfort when turning the wrist, grasping an item, or making a fist.13 De Quervain's tenosynovitis is usually associated with repetitive use of the wrist, especially wringing, thus earning the phrase "Washerwoman's Sprain." Pain may be elicited by everyday activities such as cooking, walking a pet, playing an instrument, gardening, or knitting.14
Traditionally, de Quervain's tenosynovitis is clinically diagnosed.15 A positive Finkelstein test suggests diagnosis (i.e., the patient is instructed to 1) bend the thumb across the palm of the hand; 2) bend the fingers down over the thumb; then 3) bend the wrist toward the little finger--pain on the thumb side of the wrist is considered a positive test result).9,13,14 The thickened first dorsal compartment, while made up of fascia and tendon, can be as hard as bone in these individuals.13
While radiographs are negative and not necessary for routine diagnosis, they should be obtained to rule out other conditions potentially responsible for eliciting pain.13 Radiographs may be helpful in differentiating the patient who has de Quervain's tenosynovitis from one who has osteoarthritis at the thumb CMC joint or who is suffering from both conditions.13 An MRI may also be utilized in the differential diagnosis of wrist and hand pain since its superior soft tissue contrast and multiplanar capability facilitates early diagnosis and initiation of appropriate treatment for various arthropathies and infectious conditions.11 In fact, a retrospective review of wrist MRIs indicates that de Quervain's tenosynovitis is often discovered when an MRI of the wrist is performed in suspected cases; increased tendon (extensor pollicis brevis and abductor pollicis longus) thickness and peritendinous edema are the most reliable imaging findings.15
Treatment
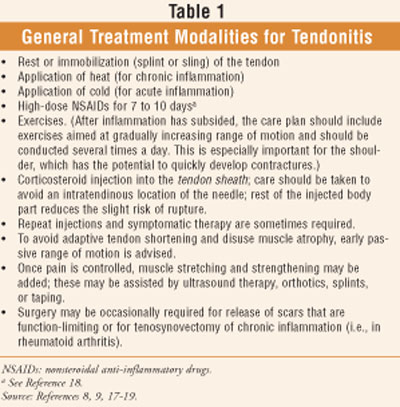
General Modalities and Nonsteroidal Anti-inflammatory Drugs (NSAIDs): General treatment for tendonitis is outlined in TABLE 1. If gout is the underlying cause of symptoms, indomethacin or colchicine may be helpful.9 Indomethacin, however, is considered a potentially inappropriate medication for geriatrics since, of all the available NSAIDs, this agent produces the most CNS adverse effects.16,17 While high-dose NSAID therapy is often indicated for tendonitis, long-term use of full-dosage, longer half-life, non-Cox-selective NSAIDs (e.g., naproxen, oxaprozin, and piroxicam) have a high severity potential to produce gastrointestinal bleeding, renal failure, high blood pressure, and heart failure in the elderly.16-18 Additionally, drug-drug interactions within the complex medication regimen, often seen among geriatric patients with multiple comorbidities, may present limitations on the treatment recommendation regarding NSAID use, even at lower doses; however, this does not imply that an older adult should be subjected to the undertreatment of pain.
Corticosteroid Injections: Stephens et al reported that corticosteroid injections relieve pain, reduce inflammation, improve mobility, and are valuable in the management of musculoskeletal conditions commonly encountered by family physicians.19 Pharmacists can assist patients by making them aware of this successful pain-relieving treatment modality and referring them for evaluation and treatment. The clinician's decision to utilize a specific medication (e.g., long-acting corticosteroid preparations such as dexamethasone acetate or methylprednisolone acetate) and frequency of injection should be guided by the following: the specific goal of the injection (i.e., diagnostic or therapeutic), the underlying musculoskeletal diagnosis, and clinical experience.19
Injections are also commonly used for postoperative pain control.19 A local anesthetic (e.g., bupivacaine) may be injected through the same needle with a corticosteroid to provide additional, rapid pain relief.9,13,19
De Quervain's Tenosynovitis: Richie et al conducted a pooled quantitative literature evaluation to determine the various reported cure rates of therapeutic modalities for treatment of de Quervain's tenosynovitis.20 The literature search resulted in the team looking at studies that reported the proportion of successful outcomes with different treatments, without a comparison to a specified control group; the study described 459 wrists subjected to one of several therapeutic modalities.20 For injection alone, the cure rate was 83%, which was much higher than any other therapeutic modality (injection and splint, 61%; splint alone, 14%; rest or NSAIDs, 0%).19 The researchers concluded that injection alone is the best therapeutic approach to de Quervain's tenosynovitis.20
While rest, warm soaks, and NSAIDs may help in very mild cases, corticosteroid injection is the preferred and definitive treatment for de Quervain's tenosynovitis.19 Improvement occurs in 70% to 80% of cases where local corticosteroid injection and a thumb spica splint have been utilized.9 Care must be taken in the procedure so as not to rupture the tendon, a rare complication of this treatment modality.9,19 It is recommended that confining infiltration to the tendon sheath and avoiding injection of the corticosteroid into the tendon (recognized as marked resistance to injection) may prevent this complication.9 A single injection permanently relieves symptoms in approximately half of patients; a second injection, administered at least a month after the first, permanently relieves symptoms in an additional 40% to 45% of patients.13 While complications from corticosteroid injections are rare, patients should be made aware of their potential risks when counseled about their therapeutic benefits.19 When periarticular, or soft tissue, corticosteroid injections are administered to patients with diabetes, these individuals should be instructed to monitor their blood glucose closely for two weeks following injection.19 To prevent de Quervain's tenosynovitis, it is suggested that patients avoid repetitive wrist and hand movements and do not pinch the thumb when moving the wrist from side to side, if possible.
Conclusion
Referral for evaluation of painful wrist and thumb pain is important since untreated pain can lead to considerable morbidity. Untreated de Quervain's tenosynovitis may permanently restrict movement of the tendons of the wrist, causing difficulty with bending the wrist, pinching, grasping, or making a fist, and may cause the tendon sheaths to rupture. With the projected growth of the aging population and the frequency with which primary care patients often report pain and reduced function associated with hand and wrist pain, pharmacists have an opportunity to refer patients for evaluation and appropriate treatment.
REFERENCES
1. WHO Scientific Group on the Burden of Musculoskeletal Conditions at the Start of the New Millennium. The burden of musculoskeletal conditions at the start of the new millennium. World Health Organ Tech Rep Ser. 2003;919:i-x, 1-218, back cover.
2. Leveille SG. Musculoskeletal aging. Curr Opin Rheumatol. 2004;16:114-118.
3. Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646-656.
4. Spies-Dorgelo MN, van der Windt DA, van der Horst HE, et al. Hand and wrist problems in general practice--patient characteristics and factors related to symptom severity. Rheumatology (Oxford). 2007;46:1723-1728.
5. Zagaria ME. Osteoarthritis in seniors. US Pharm. 2006; 31(1):20-24. www.uspharmacist.com/index.
6. Zagaria ME. Carpal tunnel syndrome: a major entrapment neuropathy in the elderly. US Pharm. 2004;29(9):30-36. www.uspharmacist.com/index.
7. Dorland's Pocket Medical Dictionary. 28th ed. Philadelphia, PA: Elsevier Saunders; 2009:833.
8. O'Rourke KS. Other arthropathies and regional musculoskeletal disorders. In: Hazzard WR, Blass JP, Halter JB, et al, eds. Principles of Geriatric Medicine and Gerontology. 5th ed. New York, NY: McGraw-Hill, Inc; 2003:1053-1070.
9. Beers MH, Porter RS, Jones TV, et al. The Merck Manual of Diagnosis and Therapy.18th ed. Whitehouse Station, NJ: Merck Research Laboratories; 2006:319-336.
10. Christian CL. Musculoskeletal syndromes. In: Barondess JA, Carpenter CCJ, eds. Differential Diagnosis. Philadelphia, PA: Lea & Febiger; 1994:811-841.
11. Jbara M, Patnana M, Kazmi F, et al. MR imaging: arthropathies and infectious conditions of the elbow, wrist, and hand. Radiol Clin North Am. 2006;44:625-642, ix.
12. Kaibara N, Yamada H, Shuto T, et al. Comparative histopathological analysis between tenosynovitis and joint synovitis in rheumatoid arthritis. Histopathology. 2008;52:856-864.
13. Meals RA. De Quervain tenosynovitis. Medscape. Updated November 16, 2007. http://emedicine.medscape.com/
14. De Quervain's tenosynovitis. MayoClinic.com. Updated April 4, 2008. www.mayoclinic.com/health/de-
15. Glajchen N, Schweitzer M. MRI features in de Quervain's tenosynovitis of the wrist. Skeletal Radiol. 1996;25:63-65.
16. Fick DM, Cooper JW, Wade We, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a U.S. consensus panel of experts. Arch Intern Med. 2003;163:2716-2724.
17. Semla TP, Beizer JL, Higbee MD. Geriatric Dosage Handbook. 14th ed. Hudson: OH: Lexi-Comp, Inc; 2009:1893-1895.
18. Table 2. NSAID treatment of rheumatoid arthritis. The Merck Manual. www.merck.com/mmpe/sec04/
19. Beutler AI, O'Connor FG. Musculoskeletal injections: a review of the evidence. Am Fam Physician. 2008;78:971-976.
20. Richie CA 3rd, Briner WW Jr. Corticosteroid injection for treatment of de Quervain's tenosynovitis: a pooled quantitative literature evaluation. J Am Board Fam Pract. 2003;16:102-106.











