US Pharm.
2007;1:73-76.
Many
women are uncomfortable discussing menopause, which involves a variety of
sensitive issues. During early menopause, women may experience anxiety,
depression, weight gain, sexual dysfunction, and stress incontinence, all of
which can be difficult to discuss. Women often refer to this stage in life as
"the change," because they associate it with a loss of fertility and youth.
Many women have difficulty sharing their concerns with and seeking advice from
a health care professional. This article provides pharmacists with strategies
for engaging women in conversations about menopause and for addressing women's
concerns regarding this transition.
Symptoms of Menopause
Menopause is
defined as the absence of menstruation for 12 consecutive months with no
underlying secondary cause of amenorrhea. In the United States, the average
age at menopause is 51.4; however, many women begin experiencing hormone
fluctuations in their early 40s. During this transition, referred to as
perimenopause, women often observe changes in their menstrual pattern.
They might notice that their menstrual flow lasts longer than usual, sometimes
exceeding seven days and resulting in a shortened length of time between
periods. At other times, they might skip one or more menstrual periods and
experience amenorrhea for 60 days or longer before their cycle resumes. This
often continues until the patient has her final menstrual period (FMP).1,2
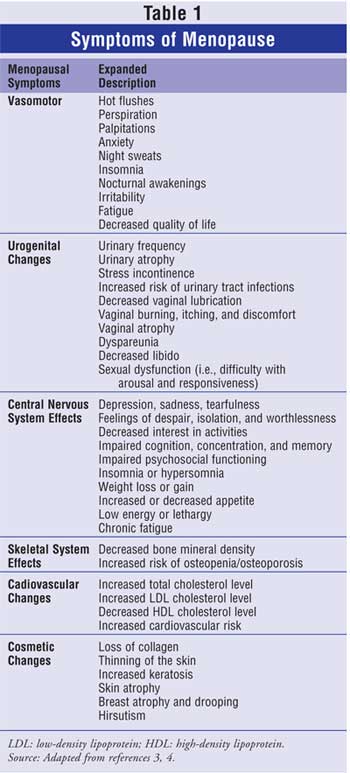
Menopause is associated with a
drop in estrogen production. Because estrogen receptors are located throughout
the body, women can develop a number of different symptoms during menopause (
Table 1).3,4 The pattern of symptoms varies from woman to woman.
The most common complaint is
vasomotor symptoms, which include hot flashes and night sweats. Vasomotor
symptoms are estimated to occur in 68% to 93% of menopausal women and are
often most severe in the first five years after the FMP. Hot flashes and night
sweats can cause disrupted sleep, daytime sedation, chronic fatigue, and
decreased quality of life. More than 50% of women who seek medical care for
menopause do so because of the severity of vasomotor symptoms. Therefore, this
symptom appears to be the one that patients find easiest to discuss.
Another symptom of menopause
that significantly impacts quality of life is physical changes in the
urogenital system. Decreased estrogen concentrations result in a thinning of
the epithelial lining of the urethra and vagina, with a corresponding
reduction of collagen and adipose tissue in the vulvar region. These changes
cause many women to experience urinary frequency, urgency, and stress
incontinence. Some women might have an increased propensity for urinary tract
infections. Vaginal atrophy also can result in vaginal burning, itching, and
discomfort. Other symptoms associated with these changes include less vaginal
lubrication, decreased libido, dyspareunia, vaginal tears, and postcoital
bleeding, which can lead to sexual dysfunction (e.g., difficulty with arousal
and/or responsiveness during sexual intercourse). Sexual dysfunction can
negatively impact personal relationships and lead to discord, anxiety,
depression, and decreased quality of life.3 Urogenital
symptoms (especially sexual dysfunction) are probably the most sensitive topic
of conversation for menopausal women. Many find it embarrassing to talk about
these problems even with their spouse, and without such dialogue, either
partner can end up feeling unattractive or undesirable.
During menopause, women might
also present with an alteration in mood. Affective symptoms include sadness,
irritability, crying spells, and feelings of despair, loneliness, isolation,
and worthlessness, as well as decreased interest in daily activities. Some
women might also experience somatic symptoms such as altered sleep patterns
(i.e., either insomnia or hypersomnolence), changes in appetite that result in
either weight gain or loss, or increased fatigue and lethargy, while other
women might report impaired concentration, memory, and cognition.4
All of these symptoms can interfere with relationships and lead to decreased
quality of life. Many women do not associate these problems with meno pause
or recognize that hormone fluctuations might be the culprit for these
problems. As women might not initiate a dialogue about these changes in mood
with a health care professional, it is important for health care providers to
initiate conversations about menopause-associated mood alterations with women.
As a result of alterations in
hormone levels following meno pause, women may also experience cosmetic
changes such as loss of collagen in the skin and less skin elasticity. Women
may notice a visible change in skin thickness, and the skin might appear more
thin and transparent. They may also notice an increase in keratosis (age
spots), especially on skin surfaces that are frequently exposed to sunlight.
Many women notice a change in hair growth and develop hirsutism, perhaps on
the lip, chin, or cheeks, as well as on other ana tomical regions. Due to
decreased skin elasticity, some women develop breast atrophy and drooping. In
addition, some women experience weight gain, loss of muscle mass, and
alterations in body fat distribution.3 Women can find these
cosmetic changes distressing and become self-conscious about their bodies.
Some women may develop body dysmorphic disorder, depression, or anxiety.
In addition to the above
mentioned acute symptoms, menopausal women also face health risks associated
with estrogen deficiency. Menopause can increase the risk of osteoporosis and
heart disease. Following menopause, women are more likely to develop
age-related diseases. Many women will realize they have passed the youthful
stage of being relatively "bullet proof" when it comes to their health, and
some might require their first prescription medication for a chronic health
condition. All of these changes can be very stressful.
As demonstrated, menopause can
negatively impact a patient's quality of life. Women are often self-conscious
about the changes occurring within their body. They might be shy or
embarrassed about talking about their health concerns. Therefore, it is
important for the pharmacist to be sensitive, responsive, attentive, and
professional when communicating with women who are experiencing menopausal
symptoms.
The Patient Interview
Pharmacists should
seek opportunities to engage women who may be experiencing perimenopause or
menopause in a dialogue concerning symptoms. They can watch for cues;
for instance, some women will make subtle comments about hot flashes. Others
might approach a pharmacist for recommendations concerning vaginal lubricants,
herbal supplements, or multivitamin formulas to help manage menopausal
symptoms. Some women might seek information concerning the pros and cons of
hormone replacement therapy (HRT). Pharmacists providing medication therapy
management services have the opportunity to explore the reproductive status of
the female patient and to screen for any symptoms of menopause when collecting
her medical history, performing laboratory tests (e.g., blood pressure,
lipids, bone minderal density), and conducting a review of systems.
When initiating dialogue about menopause
with a female patient, it is important to consider the setting of the
interview. As with all sensitive health topics, it is imperative to identify a
private counseling area where the patient will feel comfortable discussing
personal health issues. This helps promote open communication. The patient
should feel that she has the pharmacist's full attention and be confident that
she will not be overheard, judged, or interrupted during the exchange.
Next, the pharmacist should be
aware of his or her body language when discussing sensitive health topics with
a patient. He or she should project confidence and competence by being
clinically well prepared to provide pharmaceutical care to the patient. A
lapse in knowledge can cause a dip in confidence, which may cause the patient
to be reluctant to communicate. Additionally, pausing, stuttering, looking
away, or flushing because of an inability to think of what to ask or say next
can leave the patient with the impression that the pharmacist is uncomfortable
with the topic. Therefore, mental or written outlines can be useful tools for
guiding discussion.
During the interview, the
pharmacist should maintain eye contact with the patient. Leaning slightly
toward the patient will let her know that you are listening closely and are
interested in what she is saying. Notes should be taken during pauses in the
interview but not while the patient is talking. The pharmacist should let the
patient know up front that he or she intends to take some notes but should
also keep in mind that because it can be difficult for the patient to be open
and honest about her concerns, writing while she is talking may make her feel
that her concerns are not being heard or taken seriously. The pharmacist
should ask open-ended questions, encourage thoughtful responses by asking
probing follow-up inquiries, and make reflective, nonjudgmental statements
(e.g., "You have found many of these changes to be distressing").
One of the first factors that
should be addressed is the woman's reproductive stage. Is she premeno pausal
or postmenopausal? If the woman's age or menopausal status is unknown, asking
if she has experienced menopause can lead to awkwardness and embarrassment for
both parties if she merely appears older than her actual age. Therefore, it is
better to ask, "Are you having menstrual periods every month?" Posing the
question this way as sumes the patient is having normal menstruation and
allows the patient to elaborate on her menstrual cycle. If the patient says
no, follow up with probing questions such as:
• How often do you menstruate?
• How many days
does each period last?
• How many days
lapse from the start of one period to the start of the next?
• Do you
experience heavy or light flow?
• When was
your last menstrual period?
• Is there
any likelihood that you are pregnant?
• Have you had a
hysterectomy? If so, was one or both ovaries removed? Was the cervix removed?
How long ago was the procedure?
The patient's responses to
these questions will help guide follow-up questions and establish her
reproductive history. If a woman has recently developed amenorrhea, the
pharmacist should recommend an appointment with the woman's doctor for further
evaluation. She might need testing to rule out pregnancy, hypothyroidism,
hyperprolactinemia, or other endocrine disorders. In addition, a
follicle-stimulating hormone test may be needed to evaluate reproductive
status.
If it is confirmed that a
woman is experiencing menopause, the pharmacist should explore the pattern of
her symptoms and evaluate how they impact her quality of life. Since vasomotor
symptoms may be a less sensitive topic than some other menopausal symptoms, it
might be advisable to begin by saying, "Many women who experience hormone
fluctuations complain of hot flashes and night sweats. Have you noticed any
problems with temperature control?" Follow-up questions might include:
• Have you noticed any waves
of heat that begin in your scalp and move across your torso?
• Have you experienced
any feelings of being hot even when other members of your family are
comfortable?
• Have you been
adjusting the thermostat to a cooler temperature at home, even though others
in your household are cool or cold?
• Have you been wearing
lighter clothing while at home because you are often hot and
uncomfortable?
• Have you been
awakened at night due to hot flashes and sweating?
• Have you changed the
type of covering that you use at night or started kicking off the covers
during the night due to sweating?
• Are you sleeping
through the night?
• Are you experiencing
any daytime fatigue due to sleep disruption?
An open-ended probe such as
"describe those symptoms for me" or "describe your sleeping pattern" should
follow these questions.
Once a history of vasomotor
symptoms has been collected, a treatment plan can be developed. This might
include recommending nonpharmacologic interventions such as avoiding hot
environments (e.g., whirlpools, saunas), eliminating hot beverages, and
avoiding spicy foods. You might also identify a nonprescription alternative
for management such as black cohosh or soy isoflavones, or you might refer the
patient to a physician for prescription therapy such as HRT, venlafaxine, or
clonidine.
Once a rapport has been
developed with the patient, more sensitive topics such as urogenital symptoms
should be discussed. The pharmacist can ask a number of questions to explore
the patient's pattern of symptoms:
• Have you passed urine when
you did not intend to, such as when you have coughed, laughed, or sneezed?
• Are you experiencing
any vaginal dryness or discomfort?
• Have you noticed any
change in your desire for intercourse?
• Are you experiencing
intimacy problems with your partner?
• Do you have
difficulty with vaginal lubrication?
• Do you have problems
reaching climax?
• Do you experience any
vaginal bleeding after intercourse?
• Do you experience
anxiety when thinking about intercourse?
• Are you experiencing
any depression?
• Do you feel sad,
blue, or down in the dumps?
• Have you noticed a
decreased pleasure in life?
• Are you happy with
your sexual partner?
• Do you have a good
relationship with your sexual partner?
• When did you first
notice sexual dysfunction? Did this problem develop abruptly or gradually?
• Describe the emotions
you have felt since your problems with sexual function developed. For
instance, do you or your partner have anger about this problem?
It is important to ask the
patient to provide descriptive responses to each question. Because many women
are hesitant to discuss their sexuality, the pharmacist should observe the
patient, try to gauge her comfort level, and paraphrase inquiries as necessary
to keep her at ease.
Again, once the pharmacist has
collected a history of symptoms, he or she can discuss treatment options with
the patient. These might in clude Kegel exercises, vaginal lubricants, or
other interventions. In ad dition, the pharmacist may decide that the patient
requires referral to a physician for evaluation and management with systemic
HRT or vaginal HRT. If the woman is experiencing intimacy problems, she might
benefit from professional counseling. A pharmacist may not be able to address
all of the patient's health concerns regarding meno pausal symptoms, but he
or she can refer the patient to specialists who can properly assist her.
Conclusion
This article
provides information that allows pharmacists to initiate dialogues with female
patients about a sensitive topic of conversation--menopause. Using the
suggested communication strategies, the pharmacist will be able to identify
the pattern of a particular patient's symptoms and develop a management plan
for that patient.
REFERENCES
1. Menopause
Practice: A Clinician's Guide. North American Menopause Society Web site.
Available at:
www.menopause.org/edumaterials/cliniciansguide/cliniciansguidetoc.htm.
Accessed July 12, 2006.
2. Soares CN, Joffe H,
Steiner M. Menopause and mood. Clin Obstet Gynecol. 2004;47:576-591.
3. Nachtigall LE,
Nachtigall MJ. Menopausal changes, quality of life, and hormone therapy.
Clin Obstet Gynecol. 2004;47:485-488.
4. Spinelli MG.
Depression and hormone therapy. Clin Obstet Gynecol. 2004;47:428-436.
To comment on this article, contact
[email protected].











