US Pharm. 2008;33(5)(Diabetes suppl):10-16.
According to the Centers for Disease
Control and Prevention, approximately 20.8 million people in the United
States--7% of the population--have diabetes mellitus.1
Worldwide, the World Health Organization estimates 180 million people have
diabetes, and this statistic will double by the year 2030.2
Diabetes mellitus is a group of metabolic disorders characterized by
hyperglycemia, resulting from deficiencies in insulin production and/or
action. Type 1 diabetes mellitus (T1DM) results from absolute insulin
deficiency and individuals require insulin via injection or pump; this
classification accounts for 5% to 10% of cases. Type 2 diabetes mellitus
(T2DM) accounts for 90% to 95% of diagnosed diabetes cases and results from
insulin resistance in which insulin is not properly utilized by the body's
cells. For most patients diagnosed with T2DM, treatment options will include
weight reduction, exercise programs, nutrition plans, and medications (i.e.,
oral medications and/or insulin therapy).3
Glycemic Control and
Clinical Evidence
Chronic
hyperglycemia can result in microvascular and macrovascular complications.
Microvascular refers to the small blood vessels and can damage the eyes,
kidneys, and nerves; whereas macrovascular refers to the larger
vessels, resulting in heart attack and/or stroke. The Diabetes Control and
Complication Trial (DCCT) and United Kingdom Prospective Diabetes Study
(UKPDS) concluded the benefits of attaining normal glucose concentrations in
patients with T1DM and T2DM, respectively.4-7 The DCCT demonstrated
a reduction in the development and progression of microvascular complications
by 50% to 75% among patients with T1DM.4,5 The UKPDS demonstrated a
reduction in the development of microvascular complications by 25% among
patients with T2DM.6,7
Based on the DCCT and UKPDS
trials, for every 1% decrease in glycated hemoglobin (A1C), there is a 21%
reduction in death related to diabetes and 25% to 37% reduction in
microvascular complications.4-7 In addition to long-term
complications, hyperglycemia can result in acute complications, poor wound
healing, infections, and symptoms. In order to achieve desired glycemic goals,
lifestyle modifications (i.e., weight reduction, exercise programs, nutrition
plans) and pharmacological therapy will be required. It is important for
patients to take an active role in their diabetes management by monitoring
glucose concentrations.
Self-Monitoring and
Glycemic Goals
The cornerstone of
an individual's diabetes management is glycemic control, including prevention
of hypoglycemic and hyperglycemic reactions. The two primary techniques
available for assessing glycemic control are self-monitoring of blood glucose
(SMBG) and A1C measurement. Overall, SMBG allows the patient to monitor
glycemic control on a "day-by-day" basis, while an A1C measurement is a blood
test determining the average blood glucose concentration over a two- to
three-month period.
SMBG has become the gold
standard for outpatient diabetes management and short-term assessment of
glycemic control. For most patients, it is important to obtain as many points
as possible to determine an individual's constant glycemic control, depending
upon glycemic goals and medication regimen. Self-monitoring allows for
immediate feedback to the patient and is essential to achieving glycemic goals
(Table 1).3,8 In addition, self-monitoring allows the
individual to play an integral role in his/her diabetes management. Health
care professionals can assess SMBG to determine if medication adjustments or
additional glycemic monitoring is necessary.
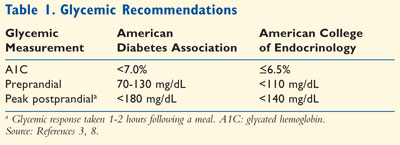
SMBG can determine if
preprandial (before a meal) or postprandial (after a meal) goals are met,
detect and prevent hypoglycemic reactions, and evaluate glycemic response to
food, physical activity, and medication changes. It is important to discuss
SMBG with all patients with either T1DM or T2DM. As a pharmacist, it is
essential to inform patients about the proper technique, interpretation of
data, and appropriate times to test glycemic response.
According to the ADA, the
following recommendations about SMBG are encouraged: 1) at least three or more
times per day among patients with T1DM, pregnant women, patients using
multiple insulin injections or insulin pump therapy; and 2) less frequently
among those on noninsulin therapy or medical nutrition therapy.3
The frequency of monitoring is determined by the needs and goals of the
patients; therefore, every patient is unique and will have a different regimen
for self-monitoring. For patients with T2DM not on insulin therapy, the
optimal frequency of SMBG is not known but should be sufficient to facilitate
reaching glucose goals.3 Certain situations may permit a patient to
monitor glycemic levels more frequently; these circumstances include
sensitivity to hypoglycemia, illness, medication changes, physical activity,
or dietary changes
Glucometers
The first blood
glucose meters (also known as glucometers) were marketed in 1971, but newer,
more sophisticated monitors have been developed. For example, the Accu-Chek
Voicemate has 20 audio features for patients with diabetes who are blind or
have visual impairment.9
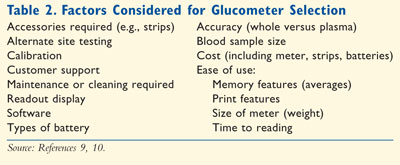
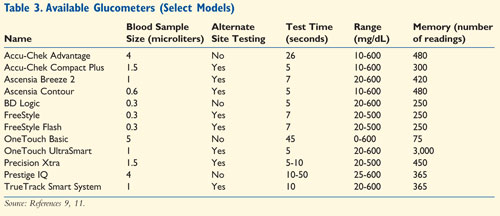
There are many factors to consider when assisting a patient in the selection of the right glucometer (Table 2 ). Depending on the retail pharmacy or store, the meter could range in price from $50 to $80.9,10 However, many manufacturers offer rebates and/or coupons. Table 3 lists some of the meters that are available in community pharmacies.9,11
Calibration
: Each glucometer has specific manufacturer's instructions for calibration
and using control solutions. For calibration, glucometers may require
insertion of a strip or chip when the monitor is purchased; other glucometers
may require proper entry of codes based on the vial of strips. If a patient
suspects erroneous readings, then a control test should be performed to verify
the glucometer and test strips. In addition, the individual should clean the
glucometer periodically. When glucometers are used properly and calibrated
corrected, glycemic results may vary by 20% in accuracy; pharmacists should
inform patients how to interpret the results.9,10 Some newer models
(e.g., Accu-Chek Compact Plus, Ascensia Breeze 2, Ascensia Contour) do not
require calibration.
Test Strips:
Test strips should be stored at room temperature in their original vial or
container. The vial should not be exposed to extreme temperatures, humidity,
or light since this improper storage may affect the accuracy. If a patient
orders the strips via a mail-order pharmacy, then the order should not be left
in the mailbox for days. The individual should check the expiration date on
the vial of strips each time a new vial is opened. In addition, it is crucial
to code the glucometer for each new vial of strips in order to get accurate
readings.
Obtaining a Blood Sample:
Obtaining a blood sample
via fingerstick may be the most difficult task for some individuals. The
patient should clean the hand with warm soapy water to increase blood
circulation. An alcohol swap can be used, but the fingertip should dry for
approximately one minute to ensure the alcohol has completely evaporated. The
lancet device is used to ensure adequate sample size and can be adjusted for
puncture depth. The lancet device should be pointed to the side of the
"tested" fingertip. Finger pads should not be punctured since this particular
area has more nerve endings and would be more painful. To increase blood flow,
the "tested" finger can be hung below the heart or massaged from the wrist up
to the tested site. Once an adequate sample is obtained, the blood should be
quickly placed on the strip.
Plasma Versus Whole
Blood: Certain
glucometer may report either plasma or whole blood (capillary) glucose
concentrations. A majority of glucometers report the glucose values as plasma
concentrations, except for the OneTouch Basic and OneTouch SureStep. Plasma
concentrations are 10% to 15% higher than whole blood glucose concentrations.
9,10
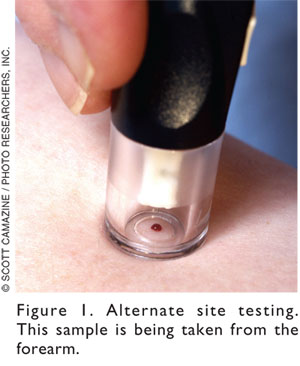
Alternate Site Testing:
Depending on the
individual's frequency of monitoring glycemic response, some patients may
complain of soreness in their fingertips and inquire about alternate site
testing. Alternate site testing (AST) is allowed at certain times and with
certain glucometers. As glucometers have become more advanced and
sophisticated, the amount of blood required has lessened. AST is less painful
due to fewer nerve endings and common sites include the palm, forearm, upper
arm, thigh, and calf (Figure 1).9,10,12 AST is reliable in a
fasting state, two hours after exercise, or two hours after meals. However,
AST locations have less capillary blood flow; therefore, these samples may not
be reflective of rapidly rising or declining glucose levels.9,10 At
any other time, the glucose levels may be rapidly fluctuating, in which
fingerstick readings would be more appropriate and reliable. When a patient
has selected a particular glucometer, it is essential to determine if the
monitor allows AST. For example, a patient can draw blood from the arm with a
OneTouch Ultra glucometer, but can check from the forearm, upper arm, thigh,
and calf with the Accu-Chek Active.9 Pharmacists have a significant
role in patient education regarding SMBG and AST.
Patient Education About
Glucometers
Pharmacists have an
integral role in educating patients about glucometers beyond calibration, test
strips, and AST. It is essential to discuss the sample size required, the time
to obtain results, memory manipulation, and replacement batteries. For
example, there are several Accu-Chek models, but each meter is not created
equal. All Accu-Chek glucometers allow AST except Accu-Chek Complete; however,
it has the largest memory capacity (i.e., holds 1,000 glucose readings) among
this manufacturer's products.9 There are many glucometers
available in community pharmacies; it is important for pharmacists in any
practice setting to remain knowledgeable about these diabetic devices.
Proper education is very
important for SMBG, especially since there are a variety of glucometers. It is
important for the patient to understand the importance of self-monitoring.
Recall demonstration by the patient would ensure understanding and allow the
pharmacist to correct any errors during this observation. Patients should be
instructed to record glucose concentrations in a logbook, with time of
medications, meals, physical activity, and any hypoglycemic reactions. This
information is valuable to the pharmacist and other health care professionals
in assessing current diabetes management and determining if a change is
necessary.
Continuous Glucose
Monitoring Systems
Over the past few
years, continuous glucose monitoring has become available as a new technology
for assessing glycemic control. The FDA has approved several continuous
glucose monitoring systems (CGMS) manufactured by Abbott Diabetes Care,
DexCom, and MiniMed; these devices continuously check interstitial glucose
concentrations throughout the day and night. CGMS does not replace the
glycemic information obtained from a standard glucometer. The CGMS has five
main components: 1) monitor, 2) glucose sensor, 3) connecting cable linking
the sensor and monitor, 4) docking station, and 5) test plug.13,14
The monitor resembles a pager
and collects the glucose information from the sensor. This component can be
attached to the patient's belt or waistline. The patient must calibrate the
monitor three to four times a day by performing fingersticks with a standard
glucometer taken at different times of the day. Special events (i.e.,
medication taken, exercise performed, or meals consumed) should be noted. For
showering, the patient may place a ShowerPak (a specially designed plastic
bag) over the monitor to prevent water damage as it is not waterproof. The
sensor consists of glucose-sensing electrodes on a polyurethane tube and rigid
introducer needle.14 The needle is inserted approximately 5
millimeters underneath the skin of the abdomen.14 The insertion of
the glucose sensor is quick and relatively painless. It is important to keep
the site of insertion sterile and the adhesive patch firmly placed to prevent
the sensor from moving. Depending on the manufacturer, measurements are
averaged every five minutes; this glucose information will be transmitted to
the monitor wirelessly.
After the glucose information
is collected (usually every three days), the sensor will be removed and the
information from the monitor will be downloaded into a computer. The monitor
is placed on a docking stand and downloaded on a standard computer using the
programmed software. A variety of graphs and charts can be printed, revealing
patterns of glucose fluctuations.
The main advantage of using
CGMS is to identify fluctuations and trends; for example, it can capture
unnoticed hypoglycemic reactions or episodes or elevated postprandial readings
in an individual. In addition, the pharmacist and other health care
professionals would be able to assess glucose concentrations in response to
dietary habits, exercise, and medications and make any necessary adjustments.
One study demonstrated the
advantage of using CGMS among patients with T1DM in detecting unrecognized
hypoglycemia.15 According to the ADA, CGMS serves as a supplemental
tool for detecting hypoglycemia unawareness, but there are no controlled
trials demonstrating improved long-term glycemic control.3 Poor
reimbursement has been the greatest barrier of the CGMS. Payers are reluctant
to provide reimbursement for patients while covering providers' time for
device application and education.13 Some insurance companies may
provide coverage or reimbursement, but certain criteria have to be met such as
unrecognized hypoglycemic reactions or suspected postprandial concentrations
with elevated A1C and normal fasting glucose concentrations.13
Continuous glucose monitoring can be reimbursed by Medicare and may be covered
by private insurance plans; inform patients to check with their insurance
carrier.
Conclusion
The prevalence of
diabetes mellitus continues to rise and is projected to increase over the next
several decades. There are a variety of agents available to health care
professional for diabetes management; it poses a challenge to pharmacists in
selecting and adjusting an individual's therapy in order to achieve short and
long-term glycemic levels. The cornerstone to diabetes management is glycemic
control. Pharmacists play an integral role in patient education regarding
glucometers. Returning to the basics by providing education about glycemic
goals, glucometers, self-monitoring techniques, and CGMS is very
important.
REFERENCES
1. Centers for
Disease Control and Prevention (CDC). National diabetes fact sheet: general
information and national estimates on diabetes in the United States, 2005.
Atlanta, GA: U.S. Department of Health and Human Services, CDC; 2005.
2. World Health Organization. Diabetes fact sheet. www.who.int/mediacentre/factsheets/fs312/en/index.html. Accessed February 21, 2008.
3. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2008;30(suppl 1):S12-S54.
4. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
5. The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342:381-389.
6. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352:854-865.
7. UKPDS 33. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet. 1998;352:837-853.
8. American College of Endocrinologists. Medical guidelines for clinical practice for management of diabetes mellitus. Endocr Pract. 2007;13(suppl 1):1-66.
9. Assemi M, Morello CM. Chapter 47: Diabetes mellitus. In: Berardi RR, McDermott JH, Newton GD, et al, eds. Handbook of Nonprescription Drugs: An Interactive Approach to Self-Care. 15th ed. Washington, DC: APhA; 2006.
10. O'Mara NM. Blood glucose meters. Pharmacist's/Prescriber's Letter. 2005;21:211208.
11. 2008 resource guide. Blood glucose monitoring and data management systems. Diabetes Forecast. 2008;61:RG31-RG48. www.diabetes.org/uedocuments/df-rg-monitors-0108.pdf. Accessed April 16, 2008.
12. Alternate site testing. www.abbottdiabetescare.com/static/content/image/asta_figure.gif. Accessed February 7, 2008.
13. Klonoff DC. A review of continuous glucose monitoring technology. Diabetes Technol Thera. 2005;7:770-775.
14. FDA. Continuous glucose monitoring system. www.fda.gov. Accessed February 20, 2008.
15. Chico A, Rio-Vidal P, Subira M,
Novials A. The continuous glucose monitoring system is useful for detecting
unrecognized hypoglycemias in patients with type 1 and type 2 diabetes but is
not better than frequent capillary glucose measurements for improving
metabolic control. Diabetes Care. 2003;26:1153-1157.
To comment on this article,
contact [email protected].











