MANAGING DRY EYE WITH RGP CONTACT LENSES
By Sam Winnegrad, ABOM, NCLEC
Course Objectives:
Upon completion of this course, participants should be able to:
- Describe dry eye syndrome and its intricate interactions with contact lenses.
- List the methods that one uses with RGP contact lenses to treat dry eye.
- Explain how Dry Eye Syndrome and its complexities require customized management approaches.
Faculty/Editorial Board:
 Sam Winnegrad is a master optician who has instructed anatomy and physiology of the eye and various other Ophthalmic courses for Roane State Community College in Harriman, Tennessee.
He has also taught for Highline College's online optician program out of Des Moines, Washington. Sam is a technical speaker for the American Board of Opticianry and National Contact Lens Examiners.
Sam holds his master's degree in Business Administration and a Bachelor's in Science, but above all, he treasures his license to practice opticianry.
Sam Winnegrad is a master optician who has instructed anatomy and physiology of the eye and various other Ophthalmic courses for Roane State Community College in Harriman, Tennessee.
He has also taught for Highline College's online optician program out of Des Moines, Washington. Sam is a technical speaker for the American Board of Opticianry and National Contact Lens Examiners.
Sam holds his master's degree in Business Administration and a Bachelor's in Science, but above all, he treasures his license to practice opticianry.
Credit Statement:
This course is approved for one (1) hour of CE credit by the National Contact Lens Examiners - NCLE, Ophthalmic Level 2, Course CTWJHI15-2
As eyecare professionals, it is crucial to thoroughly understand dry eye syndrome (DES) and its intricate interactions with contact lenses, particularly rigid gas permeable (RGP) lenses. This course will equip you with a comprehensive knowledge base, drawing insights from medical resources, research studies and practical clinical experience to provide the best possible care to patients with this common ocular condition.
Dry eye syndrome, a ubiquitous ocular disorder, affects millions worldwide. Multifaceted origins characterize the condition and can present as a chronic and often progressive ailment that can significantly impair one’s quality of life. To effectively manage dry eyes, particularly in the context of Rigid Gas Permeable (RGP) lens wear, it is essential to explore this intricate condition thoroughly.
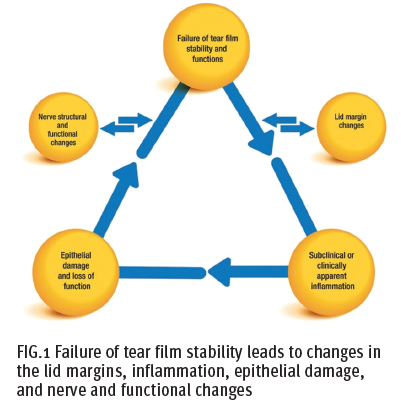
Dry eye syndrome (DES) is caused by an imbalance in the tear film, a complex structure necessary for maintaining a healthy ocular surface of the eye. The tear film coats the ocular surface, protecting the eye from the environment, lubricating, maintaining a smooth surface for light refraction, nourishing the avascular cornea, and preserving the health of the conjunctiva and the cornea. The tear film has three layers that work together to maintain stability and function (Fig. 1).
The lipid layer, the outermost component of the tear film, plays a vital role in maintaining ocular surface health and comfort. It is predominantly composed of lipids or oils secreted by the meibomian glands, which are located within the upper and lower eyelids. These meibomian glands produce a complex mixture of lipids, including cholesterol, wax esters and triglycerides.
 The primary function of the lipid layer is to act as a protective barrier for the underlying layers of the tear film. It effectively
reduces the evaporation of tears from the ocular surface, preventing rapid drying of the eyes. When the lipid layer is deficient or compromised, it can increase tear evaporation,
leading to a condition known as evaporative dry eye. This condition can cause discomfort, a gritty sensation in the eyes and blurred vision.
The primary function of the lipid layer is to act as a protective barrier for the underlying layers of the tear film. It effectively
reduces the evaporation of tears from the ocular surface, preventing rapid drying of the eyes. When the lipid layer is deficient or compromised, it can increase tear evaporation,
leading to a condition known as evaporative dry eye. This condition can cause discomfort, a gritty sensation in the eyes and blurred vision.
In addition to its role in tear film stability, the lipid layer also contributes to the even spreading of tears during blinks. This ensures that the ocular surface remains consistently moist and comfortable. Furthermore, the lipids in this layer have antimicrobial properties, helping to protect the eyes from infection.
Beneath the lipid layer lies the aqueous layer, a critical component of the tear film that is primarily produced by the lacrimal glands located in the upper outer corner of each eye. The aqueous layer is composed of a watery solution containing electrolytes, proteins and various growth factors necessary for maintaining the health of the cornea and conjunctiva.
The primary function of the aqueous layer is to provide hydration to the ocular surface. It acts as a source of moisture, ensuring that the eyes remain well-lubricated and comfortable. Additionally, this layer supplies essential nutrients to the cells of the cornea and conjunctiva, supporting their metabolic functions and aiding in tissue repair.
Inadequate production of the aqueous layer can lead to a condition known as aqueous-deficient dry eye. This can result in symptoms such as itchiness, redness, a burning sensation and fluctuations in vision quality. Moreover, the absence of sufficient aqueous components in the tear film can compromise the eye’s natural defense mechanisms against pathogens, increasing the risk of ocular infections.
The innermost layer of the tear film is the mucin or mucous layer, which is primarily generated by goblet cells located in the conjunctiva, a thin membrane covering the white part of the eye and the inner eyelids. The mucin layer is made up of glycoproteins that have a unique affinity for both water and the underlying corneal epithelium.
The mucin layer plays a pivotal role in maintaining the overall health of the ocular surface. Its main function is to ensure the even distribution of tears across the eye’s surface, promoting their adherence to the cornea and preventing irregularities that could lead to dry spots or discomfort. This even distribution helps maintain the tear film’s stability and ensures a smooth optical surface for clear vision.
Furthermore, the mucin layer aids in the spreading of tears during blinks, facilitating their uniform coverage across the cornea and conjunctiva. It also assists in the removal of debris and foreign particles from the ocular surface, contributing to eye health and comfort.
The tear film is a complex and multi-layered structure, with each layer serving distinct functions to maintain ocular health and comfort. The lipid layer acts as a protective barrier against tear evaporation, the aqueous layer provides hydration and nutrients, and the mucin layer ensures even distribution and adherence of tears. When any of these layers are compromised, it can result in various forms of dry eye syndrome and ocular discomfort, underscoring the importance of maintaining the integrity of the tear film for overall eye health.
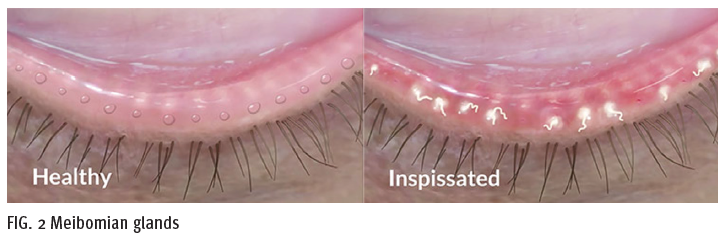
Dry eye syndrome is a complex condition with varying symptoms requiring customized management approaches. Evaporative Dry Eye constitutes the majority of dry
eye cases and is characterized by a compromised lipid layer, resulting in excessive tear evaporation. A common
underlying cause of evaporative dry eye is dysfunction of the meibomian glands—a condition known as meibomian gland dysfunction (MGD). Left untreated,
MGD can cause the meibum to stagnate in the gland, taking on the consistency of toothpaste rather than a smooth oil, leading to structural damage in the form of
gland recession and atrophy. Early treatment is vital to restoring gland function (Fig. 2). Environmental factors,
including prolonged screen time and exposure to dry conditions, can exacerbate this type of dry eye.
Symptoms of evaporative dry eye encompass stinging or burning sensations, redness, sensitivity to light, blurred
vision and a feeling of grittiness or foreign body sensation in the eyes.
Aqueous-deficient dry eye arises from inadequate tear production by the lacrimal glands. This form is frequently linked to systemic conditions such as Sjogren’s syndrome, rheumatoid arthritis, hormonal changes (especially in postmenopausal women) and medications that inhibit tear production. Aqueous-deficient dry eye manifests as persistent dryness, itchiness, redness, a sensation of a foreign object in the eye and variable visual acuity.
It is essential to recognize that many individuals experience a combination of both evaporative and aqueous-deficient dry eye with varying degrees of severity. The ability to pinpoint the specific subtype and underlying causes of dry eyes through meticulous diagnostic assessment forms the bedrock of effective treatment and management.
Recent strides in dry eye research have unveiled a deeper understanding of the condition, particularly regarding the role of inflammation in its pathogenesis. Chronic inflammation of the ocular surface can exacerbate symptoms and contribute to damage to the corneal and conjunctival tissues. This evolving understanding has spurred the development of therapeutic approaches targeting inflammation, offering promising avenues for the enhancement of dry eye management.
Dry eye syndrome is a complex disorder with various factors contributing to its development. Understanding the intricacies of tear film dynamics, differentiating between evaporative and aqueous-deficient subtypes, and recognizing the role of inflammation is crucial for effective management. For eyecare professionals who deal with Rigid Gas Permeable (RGP) lens wearers, this knowledge is essential for providing personalized solutions that improve patient comfort and eye health.
BENEFITS OF RGP LENSES FOR DRY EYES
When addressing dry eyes, especially in contact lens wear, eyecare professionals often consider Rigid Gas Permeable (RGP) lenses a promising solution. These lenses offer many advantages over their soft counterparts, underpinned by robust scientific principles and clinical evidence. In this section, we will delve into the remarkable attributes of RGP lenses and explore the scientific rationale behind their effectiveness in managing dry eyes.
One of the most distinctive and scientifically supported features of RGP lenses is their exceptional oxygen permeability. Typically composed of rigid plastics made of silicone acrylate or fluoro silicone acrylate, RGP lenses permit a substantial influx of oxygen to reach the cornea—a critical factor in maintaining ocular health and thwarting complications associated with hypoxia.
Scientific studies have unequivocally demonstrated that hypoxia, or oxygen deprivation, can lead to corneal swelling and compromise visual acuity. Due to their lower oxygen permeability (generality), soft contact lenses can contribute to this condition, making them less than ideal for individuals dealing with dry eyes.
In stark contrast, RGP lenses boast significantly higher levels of oxygen permeability, ensuring that the cornea receives an ample oxygen supply. This advantage not only reduces the risk of corneal edema but also supports the overall well-being of the cornea. Published research underscores the critical importance of oxygen permeability in maintaining ocular health, making RGP lenses a compelling choice for dry eye management.
Beyond oxygen permeability, RGP lenses present a distinct approach to tear film dynamics—a facet deeply intertwined with their efficacy in alleviating dry eye symptoms. The rigid structure of RGP lenses introduces a unique feature: the creation of a microenvironment between the lens and the cornea.
This space, often referred to as a “tear reservoir,” serves as a haven for tear exchange. It plays a multifaceted role in promoting ocular comfort and health. Scientifically, the tear reservoir facilitates the removal of debris, bacteria and inflammatory factors from the ocular surface. It acts as a dynamic buffer, preventing direct mechanical interaction between the lens and the cornea. Additionally, this microenvironment aids in the even distribution of tears, ensuring consistent lubrication throughout the day.
A study published in the Journal of the American Optometric Association highlighted the dynamic interaction between RGP lenses and the tear reservoir. It was observed that RGP lenses, with their rigid design, promoted enhanced tear exchange, resulting in improved tear film stability—a key factor in dry eye management.
Studies have revealed that RGP lenses can effectively improve tear film stability, a crucial parameter in dry eye management. This stability is paramount in preventing the quick evaporation of tears, a common issue in dry eye syndrome. By promoting tear film stability, RGP lenses significantly reduce dryness and discomfort experienced by individuals, ultimately enhancing their overall visual quality and comfort.
Moreover, real-world testimonials from eyecare professionals and patients alike underscore the practical advantages of RGP lenses for dry eyes. The ability to offer patients a contact lens option that not only corrects their vision but also addresses the underlying dry eye condition has been a transformative experience for both eyecare professionals and their patients.
Thorough preparation is essential before patients with dry eyes begin wearing RGP lenses. This preparatory phase involves more than just prescribing the lenses—it requires a comprehensive assessment of the patient’s ocular health, tear film characteristics and individual needs.
During this stage, eyecare professionals should evaluate the patient’s tear film quality and quantity, assess the overall ocular surface health, and determine the specific dry eye subtype, be it evaporative or aqueous-deficient. Then, the selection of RGP lenses can be tailored to address the patient’s unique requirements, and optimize comfort and visual outcomes.
Scleral gas permeable lenses are particularly useful in managing dry eyes as these lenses are designed specifically to avoid touching the cornea, minimizing any possible irritation and nerve desensitization, which may lead to dry eyes. Since these lenses vault the cornea completely and land on the sclera (white of the eye), they can completely change the external environment for the cornea. During scleral lens insertion, preservative-free saline is used to fill in the bowl of the scleral lens. This solution will actually “stay in place” until lens removal occurs—thus maintaining a moist environment for the anterior of the cornea. This is why it is incredibly important to use preservative-free saline, as we do not want preservatives resting on the surface of the eye without any tear exchange.
The sclera has far fewer nerve endings than the cornea, reducing the chance of irritation. Furthermore, due to their large diameter (typically greater than 15.0 mm), there is less lid interaction, which also notably improves comfort. The fluid reservoir created between the lens and the cornea is intended to fill in all of the corneal irregularities in patients with damaged or otherwise altered corneas, but it has the added benefit of providing additional hydration for the cornea. Scleral lenses should be a primary consideration for anyone suffering from dry eye who is capable of wearing lenses.
Maintaining excellent lens hygiene is a cornerstone of successful RGP lens wear, particularly for patients with dry eyes. A meticulous lens care routine ensures lens cleanliness, promotes ocular health and extends the life of the lenses.
A comprehensive lens care routine typically includes cleaning, disinfecting and storing RGP lenses. Patients must be educated about the significance of diligence and consistency in lens care practices. Providing detailed instructions and recommendations for suitable lens care products that cater to sensitive or dry eyes is essential.
Rigid gas permeable (RGP) lenses generally allow more oxygen to pass through to the cornea than soft contact lenses. This increased oxygen permeability is one of the advantages of RGP lenses. RGP lenses are made of rigid oxygen-permeable materials like silicone, which allows a significant amount of oxygen to reach the cornea. These lenses typically have higher oxygen transmissibility (Dk/t) values than soft lenses. Oxygen transmissibility is a measure of how well a contact lens allows oxygen to pass through to the cornea. RGP lenses provide a more open and breathable environment for the cornea, which helps maintain eye health and reduce the risk of complications associated with oxygen deprivation, such as corneal swelling.
On the other hand, soft contact lenses, especially those made from traditional hydrogel materials, are generally less oxygen-permeable than RGP lenses. However, advancements in contact lens technology have led to the development of silicone hydrogel soft contact lenses, which offer significantly improved oxygen permeability compared to older hydrogel lenses. Silicone hydrogel lenses are designed to allow more oxygen to reach the cornea while maintaining the comfort associated with soft lenses.
Lubricating eye drops are essential for managing dry eyes when wearing rigid gas permeable contact lenses. These drops play a vital role in maintaining ocular comfort and eye health, particularly for those experiencing dryness and discomfort associated with wearing RGP lenses.
RGP lenses, although highly effective in providing clear vision, can sometimes lead to dry eye symptoms due to their firm and less breathable nature as compared to the eye without a lens in situ. Lubricating eye drops step in to alleviate these symptoms by replenishing moisture on the ocular surface. This action helps to mitigate dryness, irritation and discomfort, ensuring a more comfortable lens-wearing experience.
Understanding the significance of lubricating eye drops is crucial for RGP lens wearers. These drops not only relieve dryness but also contribute to overall comfort. By keeping the lens surface moist, lubricating drops prevent friction between the lens and the eye, reducing sensations of irritation and redness.
Moreover, the use of lubricating eye drops is an important preventative measure. Dry eyes, if left unaddressed, can lead to complications such as corneal abrasions or infections. Lubricating drops maintain a stable tear film, thereby promoting eye health and minimizing the risk of such issues.
When it comes to selecting the right lubricating eye drops, patients should be aware of the available options. Preservative-free drops are often recommended for RGP lens wearers, as they are gentler on the eyes and reduce the risk of irritation caused by preservatives. Additionally, patients can choose between artificial tears and gel drops based on the severity of their dry eye symptoms and their preference for quick relief or longer-lasting lubrication.
Some lubricating eye drops are specifically formulated for contact lens wearers. These specialty drops are designed to work in synergy with RGP lenses, offering optimal comfort and moisture.
Integrating lubricating eye drops into a daily lenswearing routine is also crucial. Patients should apply these drops both before and after inserting RGP lenses to ensure adequate moisture and comfort throughout the day. Correct technique is essential to prevent contamination or lens displacement, so patients should be instructed to tilt their heads back, look up and gently pull down the lower eyelid to create a small pocket for drop placement.
Consistency in using lubricating eye drops is key to maintaining eye comfort and lens wearability. Encouraging patients to stick to a regular schedule ensures that their eyes remain adequately moisturized, preventing dryness and discomfort associated with RGP lens wear
Artificial tears are indispensable for individuals wearing RGP contact lenses. These drops offer relief from dryness, enhance comfort and reduce the risk of complications. It is essential for patients to understand their significance, select the right type of drops and integrate them effectively into their daily lens-wearing routine for comfortable and clear vision.
Environmental factors can significantly exacerbate dry eye symptoms and impact the comfort of RGP lens wearers. Educating patients on how to minimize their exposure to common triggers, such as air conditioning, wind and prolonged screen time, is crucial.
Practical recommendations, such as using wraparound sunglasses, using humidifiers in dry environments and employing artificial tears more frequently in challenging conditions, can significantly enhance comfort while wearing RGP lenses. By proactively addressing environmental triggers, patients can enjoy improved comfort and clarity of vision.
Proper nighttime care is paramount for RGP lens wearers, particularly individuals grappling with dry eyes. This phase of care goes beyond routine lens removal; it involves a strategic approach to safeguard ocular health and comfort during the crucial hours of rest. This section will delve into the intricacies of nighttime care and explore advanced techniques, backed by scientific insights, to maximize overnight comfort.
The fundamental step in nighttime care is diligently removing and cleaning RGP lenses. This process serves several critical purposes. Firstly, it prevents mechanical irritation that may occur if lenses are inadvertently dislodged during sleep, which can cause discomfort and damage to the corneal epithelium. Secondly, it allows the ocular surface to recover and breathe freely during the night, as contact lenses can limit oxygen flow to the cornea. This is why it is rarely recommended for patients to sleep in their lenses, even while fitting an EW modality—the complications that could ensue are almost too innumerable to mention adequately. Lastly, proper lens cleaning helps maintain lens hygiene, reducing the risk of bacterial or fungal infections.
Cleaning RGP lenses involves thorough rinsing with an appropriate multipurpose or hydrogen peroxidebased lens solution. Rubbing the lenses gently between the fingers aids in removing protein and lipid deposits, ensuring a clean and smooth lens surface. After cleaning, lenses should be stored in a clean and disinfected lens case filled with fresh solution.
For patients with dry eyes who wear RGP lenses, additional nighttime strategies can significantly enhance comfort and ocular health. These techniques are rooted in scientific principles and tailored to address the specific challenges presented by dry eyes.
Lubricating ointments, or overnight gels, are thicker and longer-lasting than traditional lubricating eye drop artificial tears. They provide a sustained protective barrier over the ocular surface, preventing overnight dryness and discomfort. These ointments are often recommended for individuals with severe dry eyes or those experiencing pronounced discomfort upon waking.
These ointments act as a semipermeable barrier, reducing evaporative tear loss while promoting epithelial healing. The ointment’s viscosity ensures prolonged contact with the ocular surface, fostering a soothing and hydrated environment throughout the night.
In specific cases, overnight lens wear may be considered an option, although it should remain a less considered option. Extended wear RGP lenses are designed for overnight use and can be worn continuously for an extended period, typically up to one month. These lenses allow patients to experience consistent vision without the need for daily removal and cleaning.
The science behind extended wear lenses involves optimizing the lens material to facilitate enhanced oxygen permeability while minimizing the risk of bacterial adhesion. This combination ensures sufficient oxygen supply to the cornea, reducing the likelihood of hypoxia- related complications while also reducing the potential for lens-related discomfort.
It is essential to note that overnight lens wear, even with extended wear lenses, requires close monitoring and adherence to strict hygiene practices to mitigate the risk of infection or adverse events. Before recommending overnight lens wear, it is important for health care providers to conduct a thorough evaluation of the patient’s eye health and lifestyle. It is crucial to fully document patient discussions and inform them of any potential risks while also advising them to contact you immediately if they experience any pain or loss of vision. A strong trust relationship is necessary when fitting a patient for extended wear lenses.
Moisture chamber goggles are also an option for individuals with severely dry eyes, particularly those who may not be suitable candidates for extended wear lenses, moisture chamber goggles offer an innovative solution. These specialized goggles create a microenvironment around the eyes, trapping moisture and preventing excessive tear evaporation during sleep. Moisture chamber goggles reduce the airflow around the eyes, minimizing the convective heat loss that contributes to tear film instability. By maintaining a humidified space close to the ocular surface, these goggles can provide significant relief for individuals with dry eyes, including RGP lens wearers.
The foundation of effective dry eye management with RGP lenses is built upon regular eye exams and consultations with eyecare professionals. Encouraging patients to maintain a consistent follow- up schedule is essential for monitoring the progression of dry eye symptoms and adapting the management plan as needed.
During these appointments, patients should be actively encouraged to discuss their dry eye symptoms, their experiences with RGP lens wear and any challenges they may encounter. This open and collaborative communication allows eyecare professionals to tailor their recommendations and interventions to each patient’s specific needs, ultimately optimizing their comfort and vision.
In conclusion, the management of dry eyes with RGP contact lenses is a multifaceted undertaking, demanding a profound understanding of dry eye pathology, lens technology, proper hygiene practices and patient education. Effective solutions exist, and with your expertise, patients can enjoy the benefits of RGP lenses while minimizing the discomfort associated with dry eye syndrome. With your dedication, you can enhance the quality of life for those seeking relief from dry eyes through RGP lens wear.



