Understanding Prism Designs for Homonymous Hemianopsia
By Charlie Saccarelli, ABO-AC
Release Date: July 1, 2018
Expiration Date: June 22, 2023
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Understand the various lens design options available for homonymous hemianopsia (HH) and how they work.
- Understand the benefits and tradeoffs of each HH lens design.
- Understand the definition of scotoma, visual confusion and prism induced diplopia.
Credit Statement:
This course is approved for one (1) hour of CE credit by the American Board of Opticianry (ABO). Technical Level 3 Course STWJHI690-3
This course builds on a previous course titled "Why You Don't Want Homonymous Hemianopsia and What You Can Do for It," which is recommended reading before taking this course. To keep things as interesting as possible, we'll be using the terms HH, hemianopsia and homonymous hemianopsia interchangeably throughout the article.
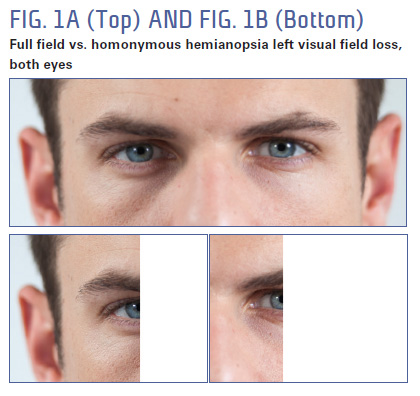
For simplicity sake, we'll be talking about a utopian "normal" case of left homonymous hemianopsia (Fig. 1), where the visual field is very clearly split directly down the vertical midline (Fig. 2), and the patient retains only the right side of their visual field. HH means that either the left or right visual field is lost in both eyes.
Also keep in mind that while this is an advanced level course for opticianry, it is not a comprehensive course on vision science, visual field loss or eye movements. This article condenses complex anatomical and physiological concepts into a sentence or two and makes simplistic generalizations to which there are many caveats. There are entire classes in optometry school dedicated to these subject matters. Opticians are not doctors, we do not diagnose nor do we prescribe but we must be knowledgeable about the design of the lens prescribed and its intended effect on HH. Please don't read this article and then attempt to debate an optometrist, neurologist or ophthalmologist about homonymous hemianopsia. It would be both inappropriate and beyond your professional reach.
 This article is going to review homonymous hemianopsia and what it's like for a patient with this condition. We will discuss the importance of considering a patient's eye and head movements in the design of eyeglassbased solutions for HH. It will cover the various eyeglass-based solutions intended to help blind-field awareness for HH. We will elaborate on the tradeoffs induced in HH lens designs due to prismatic effects such as apical scotoma, confusion and diplopia.
This article is going to review homonymous hemianopsia and what it's like for a patient with this condition. We will discuss the importance of considering a patient's eye and head movements in the design of eyeglassbased solutions for HH. It will cover the various eyeglass-based solutions intended to help blind-field awareness for HH. We will elaborate on the tradeoffs induced in HH lens designs due to prismatic effects such as apical scotoma, confusion and diplopia.
We will demonstrate the advantages of peripheral prisms and their potential benefits for both mobility and driving.
Homonymous hemianopsia is a debilitating condition related to brain injury that often cooccurs with a stroke. It's estimated to affect about one million people in the United States. Two of the most common concerns affecting the quality of life for persons with homonymous hemianopsia are driving and mobility.
OVERVIEW OF VISION & EYE MOVEMENTS
Central Vision, Peripheral Vision and Spatial Orientation: Vision is typically discussed in terms of acuity (My vision is a perfect 20/20!). But high visual acuity only occurs in a small part of our visual field. Visual acuity only measures the clarity of your central vision. While central vision is important, it's not everything. Imagine you were to take a couple of toilet paper rolls and look through the centers of them. While your vision while looking through these TP rolls is 20/20 acuity, you probably wouldn't describe it as "perfect vision" as you're bumping into everything around you.
The unsung hero of your vision is your peripheral vision. Peripheral vision detects motion and contrast in brightness (light and dark). Peripheral vision helps you detect objects in your side vision and to figure out where you are, and if there is anything that requires the attention of your sharp central vision—like a mouse scampering across the floor, or a projectile coming in your direction. It's often said that peripheral vision tells us where things are, and central vision tells us what things are.
 The chart in Fig. 3 breaks down a typical visual field into approximations of what part of your vision is higher acuity central vision (20/20-20/70), and what part of your vision is poor acuity peripheral vision (worse than 20/70). As you can see, the vast majority of your visual field is in your low acuity peripheral field of view—just used for detecting motion and contrast in brightness.
The chart in Fig. 3 breaks down a typical visual field into approximations of what part of your vision is higher acuity central vision (20/20-20/70), and what part of your vision is poor acuity peripheral vision (worse than 20/70). As you can see, the vast majority of your visual field is in your low acuity peripheral field of view—just used for detecting motion and contrast in brightness.
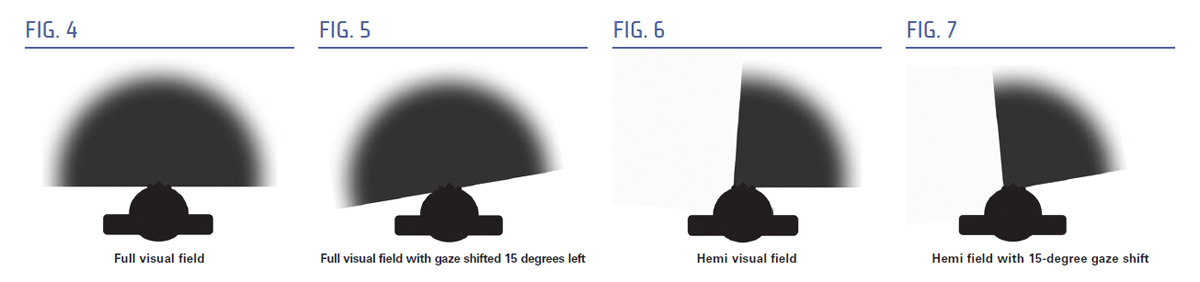
Eye Movements (Figs. 4-7): Our visual field moves as our eyes move. Your natural eye positioning is called primary gaze. But you can consciously shift your gaze. If you turn your gaze all the way to the left or all the way to the right while facing straight ahead, you can even see behind your body a bit. While you can consciously move your eyes very far from your primary gaze, your typical gaze shifts rarely exceed 15 degrees from the center with the majority of gaze shifts being 10 degrees or less. If you look all the way to the left, what you gain on one side is lost on the other side.
HH is a Visual Field Defect: The visual field loss associated with HH is most often described as the vision you have out the back of your head "nothing," or it's compared to our physiological blind spot caused by the photoreceptor free optic disc and where our optic nerve exits the retina. And while the visual field is cut in half at the vertical midline, the eye movements of the HH patient don't compensate for the loss of visual field. Visual field loss leaves patients vulnerable to collisions since they are unaware of obstacles in their blind side.
THE TRADEOFFS OF USING PRISM TO TREAT HH
 Diplopia: If you've ever had way too much to drink or have been really tired, or have certain ocular conditions; or any combination of those three things, you may have experienced diplopia. Certain eye conditions produce diplopia, such as anisometropia, where the power required in eyeglasses to correct vision is substantially different between the left and right lenses producing images of two different sizes on the retina which the brain cannot fuse into one clear image. Each of our eyes has a different field of vision, providing the brain with slightly different perspectives of the same view. When the brain cannot fuse these two images into one, then we experience diplopia, and we see an object in two places at the same time (Fig. 8). When this happens in your central vision, this is really annoying and disturbing.
Diplopia: If you've ever had way too much to drink or have been really tired, or have certain ocular conditions; or any combination of those three things, you may have experienced diplopia. Certain eye conditions produce diplopia, such as anisometropia, where the power required in eyeglasses to correct vision is substantially different between the left and right lenses producing images of two different sizes on the retina which the brain cannot fuse into one clear image. Each of our eyes has a different field of vision, providing the brain with slightly different perspectives of the same view. When the brain cannot fuse these two images into one, then we experience diplopia, and we see an object in two places at the same time (Fig. 8). When this happens in your central vision, this is really annoying and disturbing.
One of the potentially disturbing prismatic effects with the use of prisms to treat HH is central diplopia, which is very bothersome. We will learn how the placement of the prism in our peripheral visual field produces peripheral diplopia, which is well tolerated, while prism placement in our central visual field results in central diplopia, which is not well tolerated. We can use our high tolerance for peripheral diplopia when designing lenses to treat HH.
Visual Confusion: Visual confusion (double vision) occurs when the left eye sees something different than the right eye but in the same space. Normally our visual system is such that our brain fuses the slightly different view of the same thing into one clear image. But when visual confusion occurs, the view is not of the same thing—two different things occupying the same space. The brain is confused.
You might say we have double vision all the time. If you reach a hand out to each side of your body, you can see both of your hands at the same time. But if you close your right eye, you can't see your right arm. If you close your left eye, you can't see your left arm. But when both eyes are open, you can see both arms. Similarly, if you hold a finger slightly above your gaze (like where your eyebrow is), it won't really bother you. When we expand a patient's visual field, we make use of these non-bothersome areas in the peripheral visual field to expand awareness.
Apical Scotoma: A scotoma is a missing part (gap) in our visual field. Macular degeneration is known as a central scotoma. Our physiological blind spot is a scotoma. Anywhere that visual field is perceived as missing can reasonably be considered a scotoma. The missing field from hemianopsia is a scotoma. Scotomas can also be created. If we put surgical tape on a pair of glasses, we create a scotoma.
An apical scotoma is the image jump experienced as you look through the apex of a prism. The missing area between the last ray of light not in the prism and the first ray of light in the prism can be quite sizeable when high powered prisms are used, and quite obtrusive if they are placed in the important central area of your vision.
The image jump experienced at the edge of a round bifocal is one form of an apical scotoma. A +3.00 add in a 22 round bifocal segment produces a 3.3 prism diopter image jump. This translates to roughly 1.6 degrees of apical scotoma. The prisms used in hemianopic lens designs are often upwards of 20 prism diopters, which would create an apical scotoma of up to 10 degrees of gap in the visual field. We will discuss the implications of this as we review the various lens designs.
WHAT ARE WE TRYING TO FIX?
Designing eyeglasses without considering a patient's lifestyle needs is a bit myopic (pardon the pun). Two of the primary complaints hemianopsia patients have are driving and mobility.
DRIVING
Determining eligibility and the ability to drive is largely a legislative one. Visual field requirements are established by states. Some states have a path from homonymous hemianopsia to licensure. Some states have no path. Some states just don't care about the visual field at all. Fixing these inconsistencies is beyond the scope of this paper. Clearly, our goal is to help HH patients expand their field of vision and increase awareness of what lay in their blindside. In some states, this will increase their field of vision enough to allow them to obtain a driver's license.
A MODEST PROPOSAL REGARDING MOBILITY
In assessing the potential benefits of lens designs, I propose two truths. 1. If you see something, you are less likely to trip over it or run into it, and 2. If you trip over or run into fewer things, you could call that improved mobility.
As proven by the Flat Earth Society (pardon my audacity if you're a member), few things are universally accepted as truth. But moving forward in assessing lens designs for HH, this writing will hold the above proposed truths to be self-evident. And building on those truths, it's safe to say that giving the patient more awareness of their blind side can improve mobility. That is the goal in designing lenses for HH—to create more awareness of the blind side. How do we do that?
HOW TO ASSESS LENS DESIGNS FOR HH
To measure the efficacy of lens design for hemianopsia, we want to conceptually validate the truths above, and we want to validate them with the patient's eyes at various positions of gaze so we can simulate the dynamic component of vision. Since 90 percent or more of eye movements are 15 degrees or less, we'll assess each lens' function at primary gaze, 15 degrees gaze right and 15 degrees gaze left. We will do this in dramatic fashion with simulated graphics and then in a more scientific fashion with charts of anticipated visual field measurements. We're also going to describe the process the patient must go through to view something on their blind side.
DRAMATICALLY SIMPLIFIED SIMULATED GRAPHICS
Welcome to the monochromatic petting zoo that exists solely on a single horizontal plane. Life isn't like this. In life, you have some high, some low, some large, some small, some near, some far. In our petting zoo, we have a kangaroo-sized spider and a goatsized frog. A kangaroo-sized spider probably shouldn't even be at a petting zoo anyway. This simplification is to simulate lens designs for HH and their utility along the horizontal plane of the visual field.
Fig. 9 represents a full petting zoo as seen by a patient with a full visual field when they are looking at the goat. The arrow represents the primary position of gaze. The graph in Fig. 9b is a graphical representation of a full visual field. The purple is the left eye's visual field, and the red is the right eye's visual field. The overlap is the binocular visual field, and the green dot in the center represents the small area of central vision where we're capable of our best visual acuity.


This is the petting zoo as seen by a patient with left homonymous hemianopsia when they are looking at the goat (Fig. 10a). Notice the gaze (arrow) is shifted slightly left to capture the goat in the visual field. The graph in Fig. 10b shows a left hemianopic visual field. The red is the right eye visual field, and the darker color is the binocular visual field of both the left and right eyes.

LENS DESIGNS
The lens designs for hemianopsia can be split into four categories: 1. Yoked prisms. 2. Yoked sector prisms. 3. Unilateral (one-sided) sector prisms, and 4. Peripheral prisms.
YOKED PRISM (Shifts field but no field expansion)
All of our training in opticianry says yoked prisms cancels out. But a considerable body of optometry research on concussions, TBI and stroke care find yoked prisms are beneficial for gait, posture and stability. But we'll save that for another day. Right now, we're reviewing lens designs to help with visual field expansion for homonymous hemianopsia. So let's see if yoked prism in our lenses creates field expansion.
Here we have our left HH hemi field, and we're admiring a lovely breed of monochromatic goat (Fig. 11a).
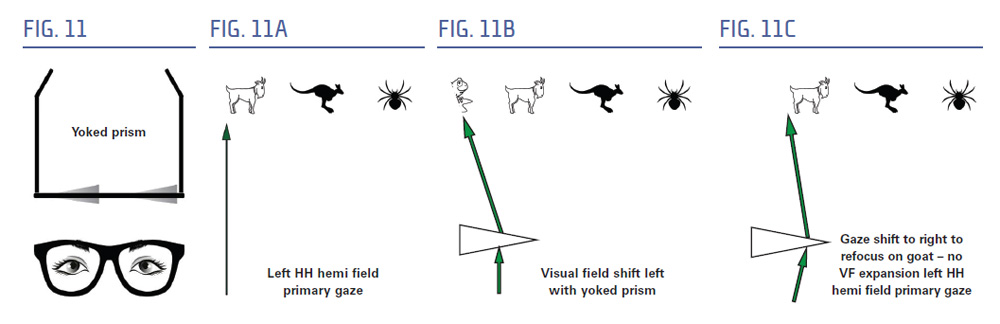
We put a yoked prism (Fig. 11) in front of our eye to shift the field of view so that we can see into our blind side to the left. Now we see the nose of a frog (Fig. 11b). Excuse us, but we weren't done looking at the goat. What do we do?
We shift our eyes right, to look at the goat (Fig. 11c). In doing so, we offset the shift offered by the prism, rendering it useless from a field expansion perspective. This effect will be the same at all positions of gaze.
YOKED SECTOR PRISMS
(Field substitution with apical scotoma)
A yoked sector prism (Fig. 12) is comprised of a prism in each lens, usually somewhere between 12 and 20 diopters, with the base in the direction of the blind side, and the prism off into the blind side by a few millimeters. I know what you're thinking...how does a prism work to expand visual field if the patient can't see it? That's kind of like putting glasses on the back of your head! Let's see how that works.
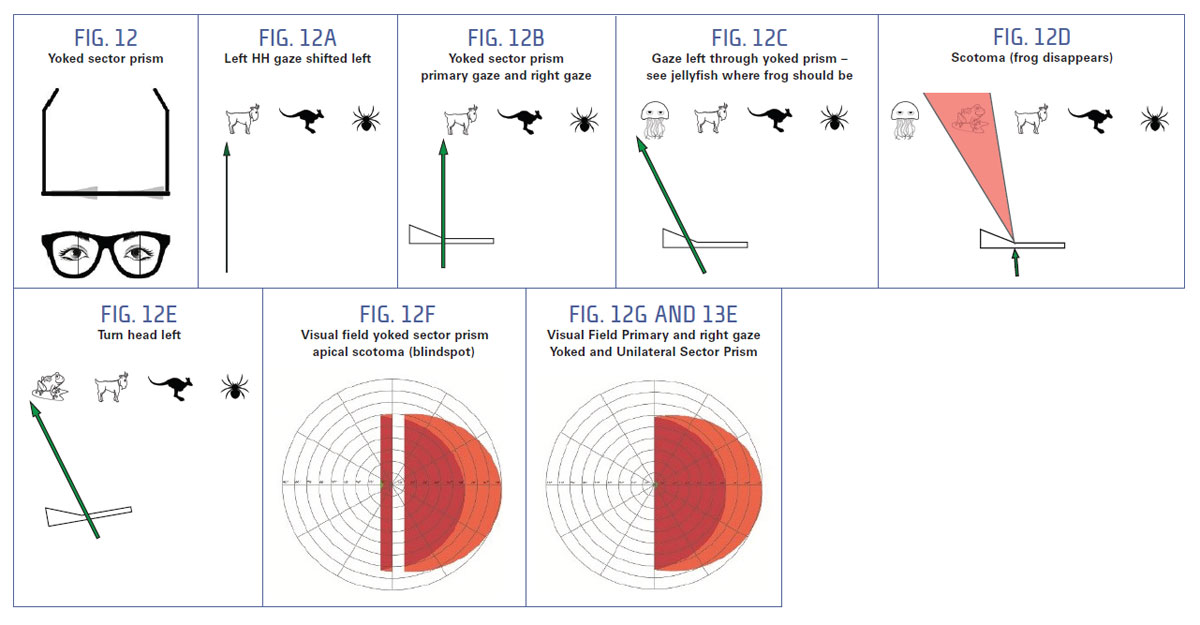
Fig. 12g shows our regular left HH visual field. Now let's put a yoked sector prism in the lens to demonstrate what we'll see using our primary and right gaze versus left gaze into the prism and the blind side.
Here's our view through the yoked sector prism (Fig. 12a). All good, right? With our eye at primary gaze fixation, we still see a beautiful monochromatic goat. There will be no change as we gaze to the right, the kangaroo and the spider will be in our visual field.
But when we turn our eyes left to look at the frog, what happens? (Fig. 12b)
This is clearly not a frog. This is a jellyfish (Fig. 12c). How did it get there, and how do we get to the frog? Ok, what is this? We're trying to look at the frog.
The disappearing frog is the result of the apical scotoma (Fig. 12d and 12f), a gap in vision that occurs as the eye looks through the last ray before crossing the prism apex (comes from the front of the frog), and the first ray deviated by the prism (comes from after the frog). The visual effect is a disappearing frog. Imagine if that frog were a stop sign or a telephone pole. You would drive or walk right into it.
So how do we see the frog? That's our goal here: You must turn your head to look at the frog, so you're looking through the portion of the lens that has no prism (Fig. 12e).
Since the same type of lens is fit in both eyes, we can simulate binocular vision using a single lens. When we get to the other types of lenses, we will split the function of left and right.
UNILATERAL SECTOR PRISM
(Expands the field of view but produces apical scotoma, central diplopia and visual confusion)
Unilateral sector prisms are typically positioned base out on the side of the field loss, a few millimeters into the blind side. Unilateral sector prisms do offer visual field expansion, but at the cost of uncomfortable diplopia in central vision. Diplopia in central vision can cause a few different things depending on the patient, but none of them are particularly positive. First, it can cause fusion, which means the patient's eye muscles are strong enough to merge the prism image and the non-prism image, thereby eliminating the field expansion. Second, it can cause suppression, where the brain blocks signals from one eye; just turns off due to the discomfort. Third, it will cause the patient to adjust their neck so they can avoid looking into the prism, which defeats the purpose of the field expansion. Unilateral sector prisms go by many names: side vision awareness glasses, rekindle prisms, button prisms, onufryk prisms to name a few. So let's look at the lens. Since each eye gets a separate treatment, we will analyze monocular effect before analyzing the binocular effect.
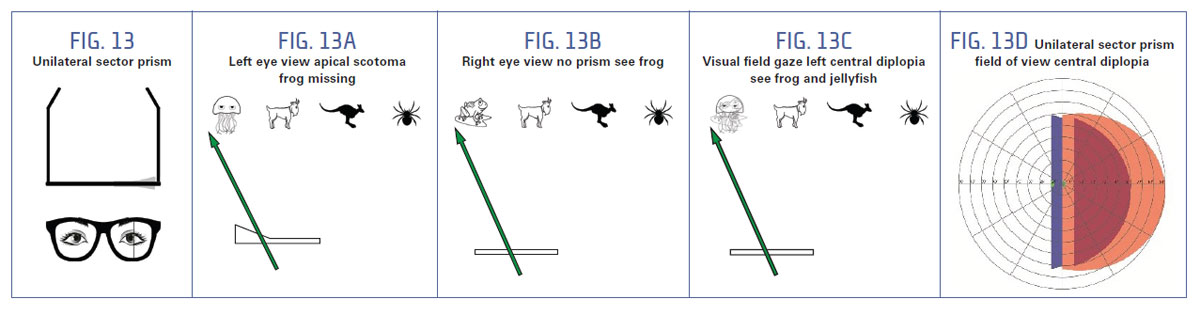
Here's our left eye view through a sector prism (Fig. 13a). It has the same apical scotoma as the yoked sector prisms, but it only affects one eye. So with the left eye, when we turn our eye to look at the frog, we see a jellyfish but don't see the frog (due to apical scotoma).
Here's our right eye, with a standard lens, no prism (Fig. 13b). When we gaze to the left, we see the frog. Good!
But we have two eyes. The left sees a jellyfish, and the right sees a frog. That's not good. We just want to see a frog, not a frog-fish (Fig. 13c). So how do we avoid the frog-fish? We just want to look at the frog. Well, the patient either needs to close one eye or turn their head to look at the frog.
PERIPHERAL PRISMS
Peripheral prisms work differently than the sector prisms. Rather than sitting in the "what things are" in the central part of the blind area, they are placed in the "where things are" in the peripheral portion of the seeing area. Because of this positioning, the patient is given a highly tolerable form of double vision, aka visual confusion, in their peripheral vision that results in a significant amount of visual field expansion. These prisms are fit in two different variations: oblique, which brings in the field from the visual midline, and horizontal prisms, which bring in field from the top and bottom of the midline leaving the central visual field free of diplopia, confusion and apical scotoma. Because our petting zoo really only exists along the midline, we'll display the effect using monocular oblique prisms and then describe the differences afterwards.
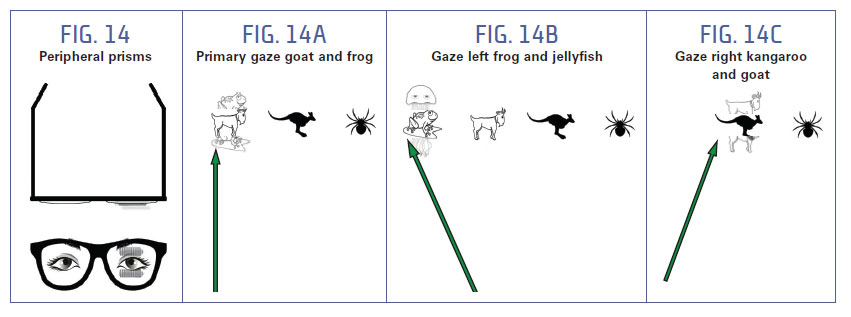
Fig. 14a shows the field of vision with our primary gaze. At primary gaze, the patient will have an awareness of the frog to the left in their peripheral vision.
Fig. 14b shows the field of vision with our left gaze shift. The patient will have an awareness of the jellyfish to the left of the frog in their peripheral vision.
Fig. 14c shows gaze right. When the patient looks at the kangaroo, they will have an awareness of the goat to the left of the kangaroo in their peripheral vision.
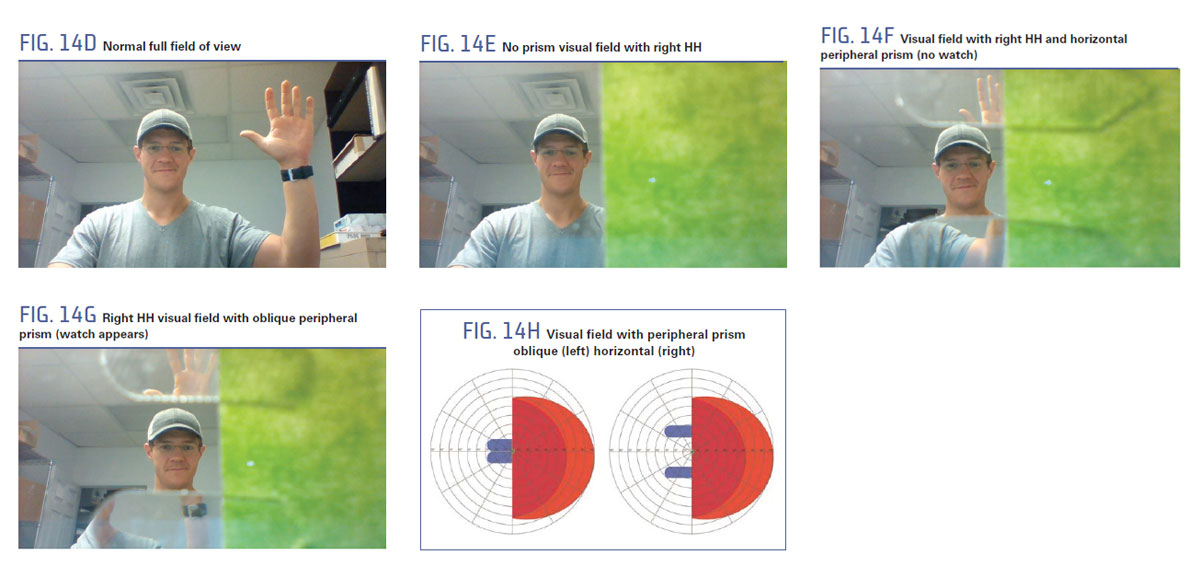
FLEXIBILITY OF FIELD AWARENESS WITH PERIPHERAL PRISMS
The coolest thing about peripheral prisms is that by angling the prisms different ways, you can angle the field awareness in different directions. By positioning the base of the prism out, the field can be expanded straight out (Fig. 14f). This has been found to be the best for mobility. But by angling the prisms with the bases toward the center, the visual field can be expanded centrally instead. This would be especially helpful if a patient were driving with hemianopsia and would need their visual field to expand outside the windshield (Fig. 14g).
NOW WHAT?
Doctors often end up prescribing eyeglasses for homonymous hemianopsia. As an optician, knowing about these types of lenses could make you a valuable resource for specialty optometrists and ophthalmologists who know what kind of glasses their patients need, but not where to get them. It's safe to say there are at least 1,000,000 homonymous hemianopsia patients in the U.S., and many of them can be helped by glasses. As opticians, designing lenses is our forte. Learning about specialty lens treatments and low vision aids helps us help doctors provide solutions for the vision challenges facing an ever growing population beset by age and illness related vision disorders.



