
By Thomas H. Clark O.D.
Part 3 discussed the effect of angle Kappa on PAL fitting. Part 4 addresses the effect of the dominant eye and alignment error on PAL success.
DOMINANT EYE EFFECT – A CONFOUNDING FACTOR
A patient’s adaptive response is for the dominant eye to center on the clearest portion of the segment in the lens in front of the dominant eye. If the lenses are incorrectly aligned, the non-dominant eye’s visual axis will now fall outside the umbilic. That results in a head or eye turn to make near vision clear. That leaves the non-dominant eye with unclear, distorted vision, the result of coma and surface astigmatism. The amount of alignment error and visual disruption for the non-dominant eye will be the total linear error for both eyes dependent on the value of that patient’s angle Kappa, see Figure 8
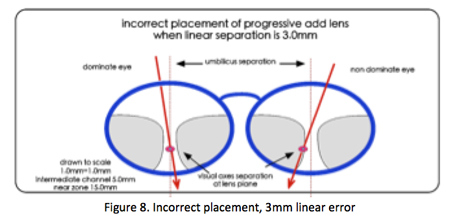
As the linear error increases the cone of clear foveal and parafoveal vision falls farther from the umbilic causing even more blurred vision. Figure 9 shows the effects of the incorrect placement of 3.0 and 5.0mm segment placement.

BINOCULARITY AND INTOLERANCE
This blurred image in the non-dominant eye causing stereoscopic disruption is one of the causes for visual discomfort resulting in high redo and non-adapt rates.
Blur suppression and stereoscopic disruption have been observed and studied extensively with the technique of mono vision contact lens fitting. This is the technique of fitting the dominant eye with a full distance prescription and the non-dominant eye with a near prescription, causing blur at distance. Studies show that 40% to 50% cannot suppress the blurred image or tolerate the stereoscopic disruption caused by the blur in the non-dominate eye at distance. This results in a patient’s rejection of this system. (2)
Therefore, the range of intolerance and rejection of a patient to their progressive add lens can be caused by the amount of visual axes misalignment, a patient’s intolerance to stereoscopic disruption and the patient’s inability to suppress those images.
LINEAR PD/VISUAL AXIS DIFFERENCE IN A POPULATION BASE OF 200 PAL WEARERS
What is the linear measurement difference (the error) if angle Kappa affects centering? In other words, can the error of centering be quantified in relation to measured pupillary distances?
For the purpose of this study, the definition of linear error is the difference between the patient’s pupillary axes separation at the lens plane and the patient’s visual axes separation at the lens plane fitting points (Figure 8).
This study reviewed 200 randomly selected patients in my practice that had previously been prescribed and wearing progressive add lenses.
Two measurements had been taken when these patients were fit with PALs
- A near and far pupillary distance (PD) measurement using a corneal reflection-type measuring device
- A near and far visual axis separation measurement with a prototype-measuring instrument based on my patent: Visual axis and alignment measurement system and method of using same, US 7628489.
This interactive, patient operated instrument measures the separation of the patient’s visual axes at the approximate lens plane using the patient’s subjective feedback. These measurements were compared and the difference was noted as a linear error (Figure 8).

This study shows that using a corneal reflection measurement for PAL segment separation would have resulted in having the patients’ visual axes and their PAL segment misaligned by 0.0 mm to as much as 6.0mm, half with an error of 2.5mm or more. In fact, 33 percent of these patients had a linear error, a difference between the measured PD and visual axis separation distance of at least 3 mm or greater. How disruptive is this linear error?
A 2mm linear PD error in a pair of lenses (vertex distance of 15mm) will force the patient to move his gaze 4 cm to clearly view from one near target to the other at a viewing distance of 16 inches.
How a patient’s unique visual system handles this visual acuity imbalance or disruption is what will determine if the progressive add lenses will be tolerated or not. A patient’s adaptive response could range from the suppression of the blurred image at one end of the scale to having a high sensitivity to stereoscopic disruption and rejecting the progressive Rx at the other.
All present methods and instruments from a PD ruler, corneal reflection as well as digital instruments locating the pupillary reflex have one basic commonality – they all use external measurements to determine PAL segment separation and placement. Digital devices, however, get the effect of frame fit on monocular PD correct because they include frame fit on the nose. That aside, the biometric issue of angle Kappa exists in almost our entire patient base. Therefore, external measurements will tend to be slightly to highly inaccurate.
This new information suggests:
- An opportunity for a re-evaluation of the value of the present methods and instruments in regard to accurate progressive placement.
- A need to develop methods to measure the actual visual axes separation at the lens plane of patients Rx. (fitting point separation).
- The use of distance and near, visual axes separation values, as the gold standard monocular “PD“ fitting point separation used to order progressive add lenses. This would make the progressive umbilic separation the same as the visual axes separation measurement at the lens plane as the primary measurement for the Rx.
- The need for a verification method and instrument to determine the correct progressive centering.
Part 5 will introduce devices and methods to obtain visual axes separation measurements.
Dr Thomas Clark OD, http://www.willistonoptometrist.com/
For further information on this measuring system contact iPCapital Group
www.ipcg.com













